
Shin splints, also known as medial tibial stress syndrome (MTSS), is a common condition defined by pain along the shin bone (tibia). This is one of the most common lower body conditions, comprising 16% of all running-injuries. It is particularly common in athletes in military recruits.
Shin splints are considered a clinical pain syndrome. This means that there is no consensus on exactly how it occurs. Rather, there are a few correlated symptoms that appear together:
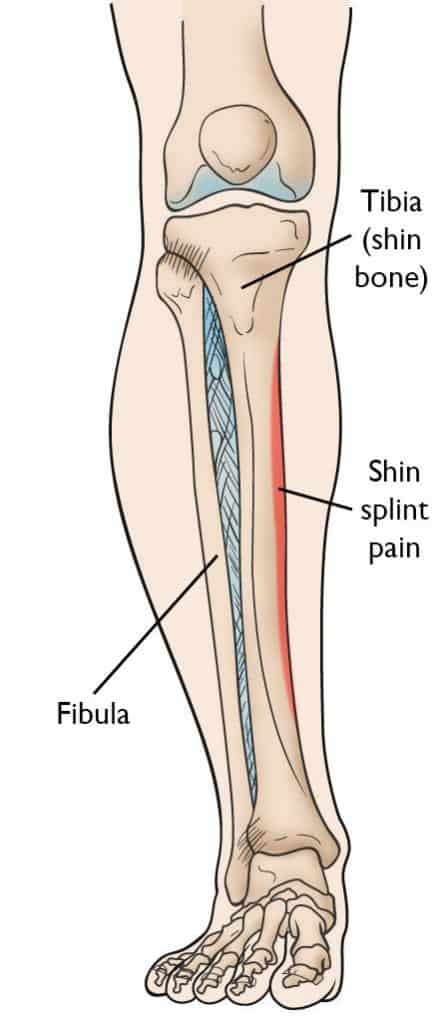
It’s important to note that imaging is not useful for diagnosing shin splints. Multiple studies have shown that x-ray, ultrasound, CT scan or bone scans are not sufficient to diagnose MTSS. However, imaging can help rule out the possibility of other conditions, such as a stress fracture.
There are two main theories for why medial tibial stress syndrome develops:
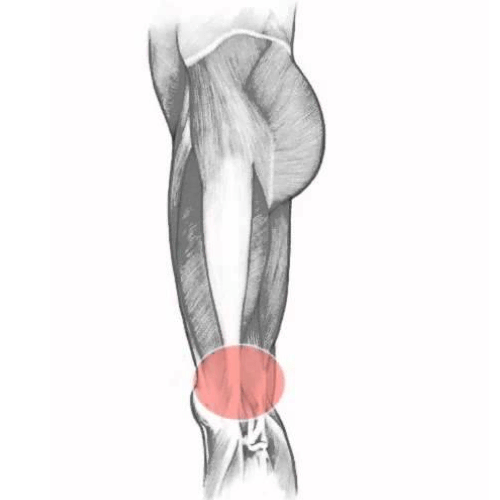
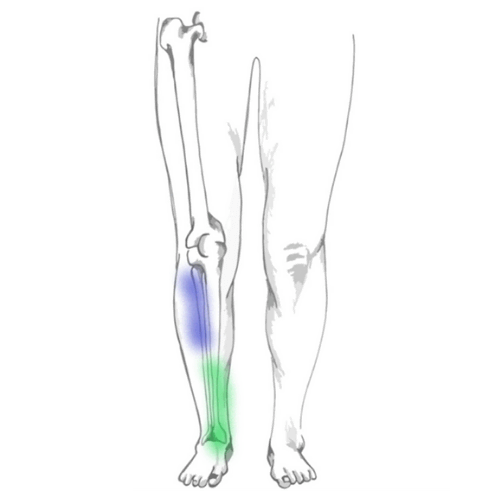
Let’s start with fasciopathy. There is thick connective tissue, known as fascia, that attaches to the posteromedial border of the shin (i.e. the site where shin splints occur). The muscles within the deep posterior compartment of the lower leg – namely flexor digitorum longus and tibialis posterior – can tighten the fascia when they contract. This traction force can pull on the attachment site on the periosteum of the tibia and cause symptoms of medial tibial stress.
Bone overloading is a recent proposed mechanism for the development of shin splints. At the tibial border, there is evidence to show decreased bone mineral density in symptomatic individuals. Once bone mineral density improves, symptoms also improve. In some cases, the bone at the injured area showed signs of impaired repair. With the high impact forces and repetitive nature of running, it is logical that these forces can over-stress bone and lead to pain.
Its plausible that either mechanism or both together can lead to the development of medial tibial stress syndrome.
The incidence of shin splints tends to be higher in individuals with certain risk factors. A systematic review found the following five factors predicted a higher risk for the development of MTSS:
It’s unclear why females have a higher prevalence of shin splints, but some researchers believe it relates to running biomechanics. In military recruits, they found that women were at higher risk of MTSS from over-striding to keep up with men’s marching cadence.
A higher body mass index (BMI) was found to be a significant risk factor. This is not surprising, considering that the leading theory for MTSS is a bone stress injury. High body weight leads to higher forces on the bone during running and can contribute to the development of shin splints.
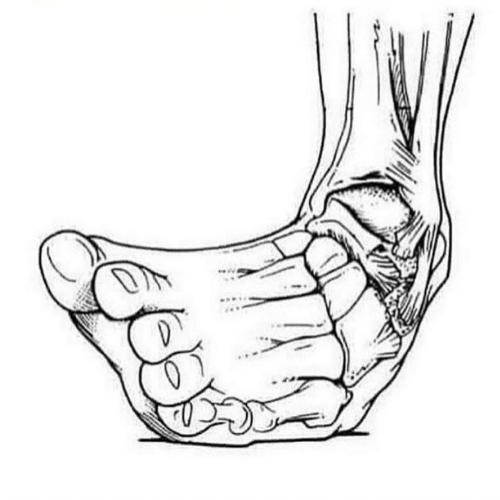
The navicular bone is an important bone in the foot that helps form the arch and allows you to walk. When the navicular bone drops towards the floor, which is typical for someone who is flat-footed, the arch also collapses. This can lead to altered gait mechanics that contribute to shin splints.
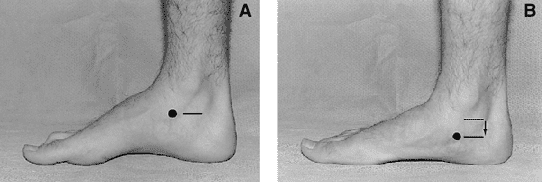
There are several ways to mitigate this risk factor. The primary method is to work on foot control and strengthening of the foot intrinsic muscles as well as the tibialis posterior muscle, which connects to the navicular and helps support the foot arch. Orthotics can help control navicular drop by providing arch support.
It’s no surprise that a previous injury leaves you susceptible to future injury. This is a common risk factor in nearly every musculoskeletal condition.
Multiple studies have found this link, yet it is unclear why this particular movement pattern is present in individuals with MTSS.
Shin splints can take a long time to fully recover. Studies suggest that it can take upwards of 3 months to run for 20 minutes without pain. Full recovery can take between 9-12 months or more depending on the person and the length of symptoms.
The cornerstone of any treatment is a proper understanding of the condition. There are a few foundational management strategies for medial tibial stress syndrome, including:
The first step to recovery is to manage the forces on the bone so it can adequately repair itself. there are some general guidelines to help manage these loads. One common approach is to limit any increases in volume, frequency or intensity by no more than 10-30%, depending on the individual. This can help you avoid large spikes in training loads that negatively impact bone remodelling.
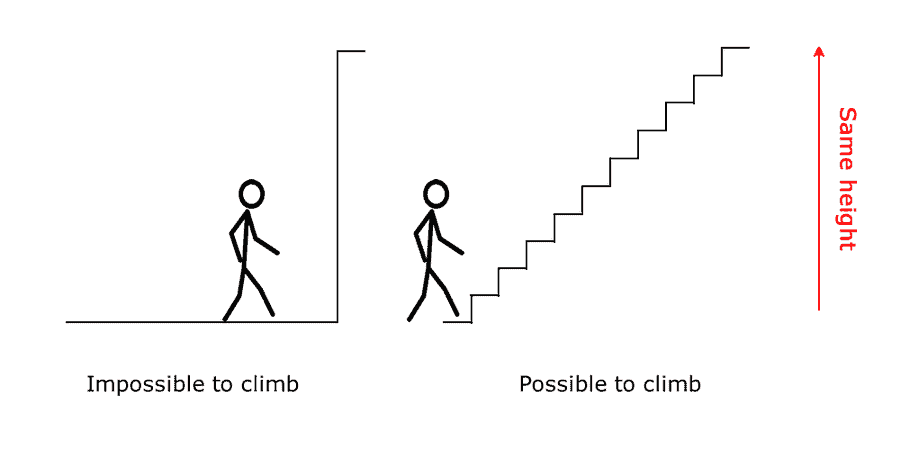
There is a concept in rehabilitation called graded exposure. Graded exposure is the slow and deliberate introduction and increase in a stimulus – in this cases load – to induce adaptation in a specific tissue (such as bone) or individual. A carefully constructed rehabilitation program can achieve this balancing act to maximize recovery.
A graded-exposure program combined with exercise has been shown to be effective. Most studies combine a tibial loading program with plantar flexor strengthening. The plantar flexors include the calf muscles (the soleus and gastrocnemius). Strengthening the lower leg can help improve the resiliency of the body to withstand the forces applied to it during jumping and running activities.
We typically advise keeping the pain score under a 2 out of 10 when performing exercises. A small amount of discomfort is acceptable, but the pain should subside when the exercise is finished.
In some individuals, changes running gait patterns can substantially reduce symptoms. In our experience, we’ve seen that changing over-striding and foot position during running (i.e. reducing tibial rotation on landing) can lead to symptom reduction.
Managing symptoms is useful to help individuals participate in an active recovery plan without fear or hesitation. While we encourage minimizing modality-based treatment, especially since it can mask symptoms and make it more challenging to fine-tune your load management program, it can be useful in certain cases. When symptoms are severe in the initial stages and the patient is not able to fully participate in an active program, modalities – such as manual therapy, acupuncture, ice and shockwave – can help.
As in most conditions, a multi-modal approach that is informed by the research evidence but that is tailored to you is the best option.