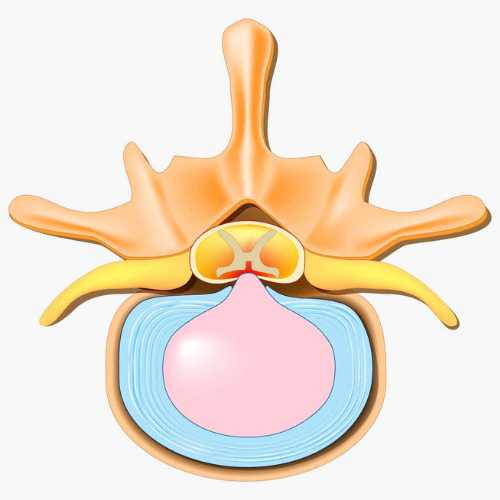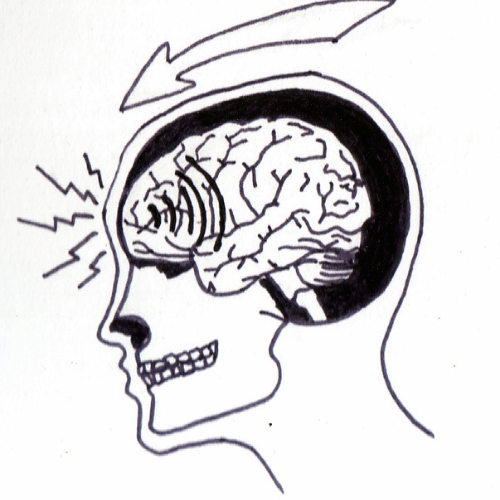

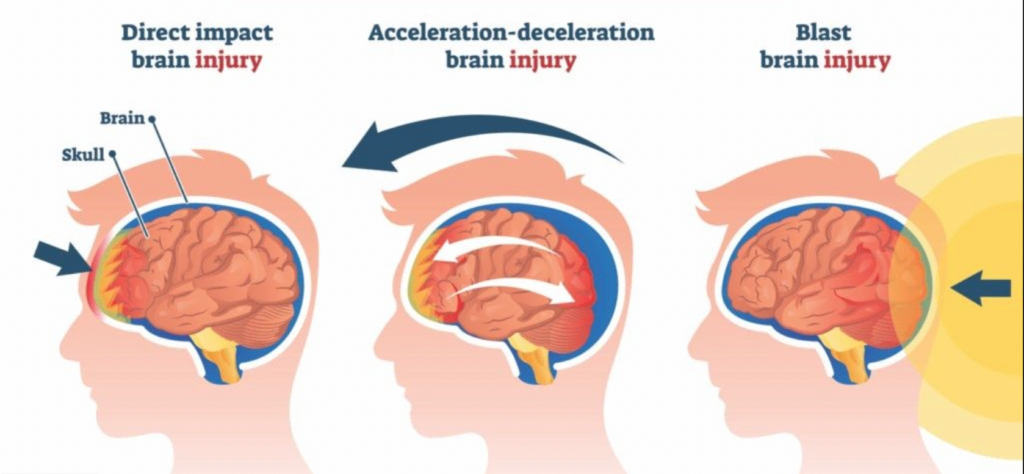
A concussion is often defined as the immediate and transient symptoms of a mild traumatic brain injury induced by biomechanical forces. This can be from a direct blow to the head, face, neck, or elsewhere on the body with an impulsive force transmitted to the head. Acute signs of concussion indicate functional disturbances rather than any specific structural injury, as a result no abnormality is seen on standard imaging.
Concussions are considered one of the most complex injuries in sports medicine to diagnose, assess, and manage. A significant majority of concussions occur without loss of consciousness or obvious neurological signs and there is currently no perfect diagnostic test for them. As a result, in all cases of suspected concussion, the individual should be removed from the playing field and assessed by a licensed health care provider1.
It is important to know that an acute concussion is an evolving injury; some symptoms may appear instantly, while in other instances, they may not appear until minutes or hours after the event and can rapidly change. Concussion can vary greatly, but their presentation commonly includes:
Approximately 80 to 90% of concussions resolve within 7 to 10 days and symptom resolution typically follows a sequential course, however in some cases symptoms may be prolonged1.
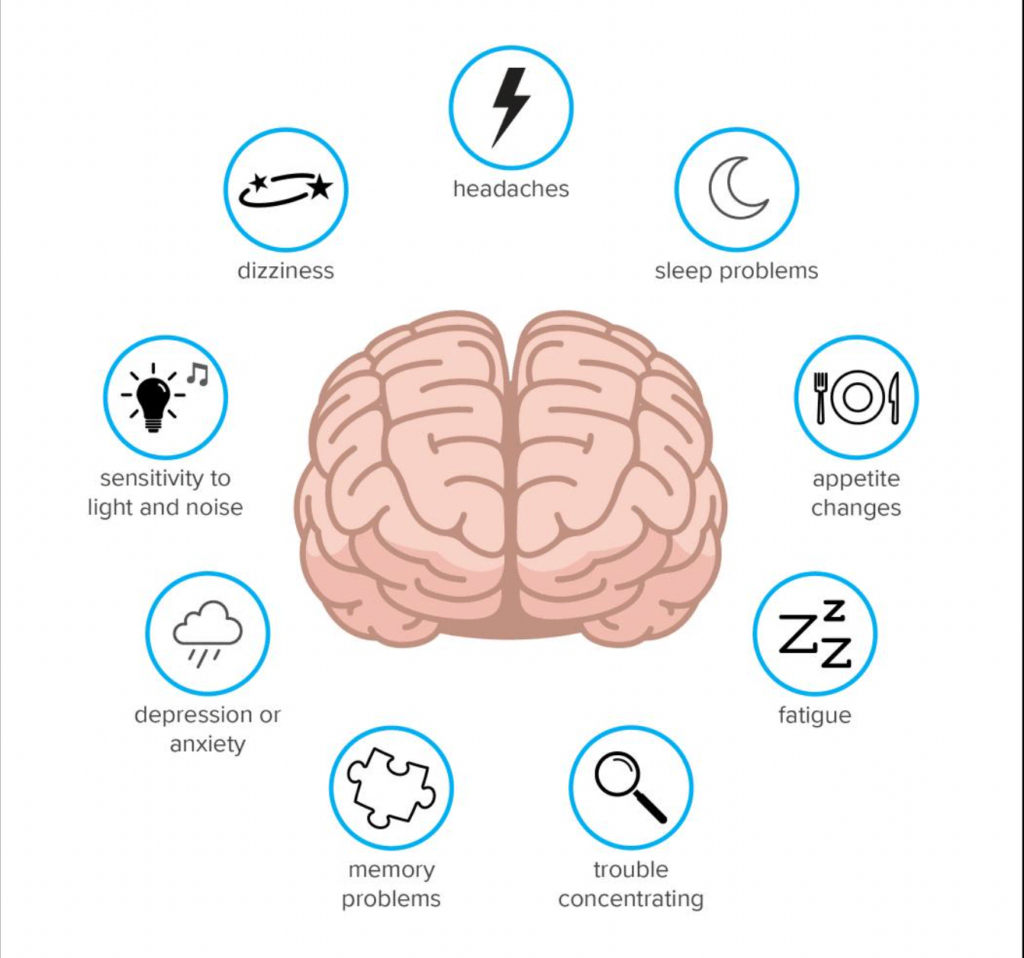
When symptoms persist longer than 7 to 10 days, this is referred to as ‘Post-Concussion Syndrome’. A majority of post-concussion syndrome cases resolve within three months, however there have been cases of symptoms lasting up to a year. There is no proven correlation between injury severity and the likelihood of developing concussion symptoms or post-concussion syndrome. There is evidence that rather than strict rest, participating in moderate levels of physical and cognitive activity can be beneficial for the management of post-concussion symptoms2.
Concussions do not represent a single consistent pathology, but rather a wide array of symptoms that must be assessed and treated in an individualized manner. A clinical assessment is required to identify any deficits and a treatment plan will target those processes specifically.
In the past, concussed individuals were usually prescribed rest until they became symptom-free. The basis for physical and cognitive rest is that rest may play a role in easing discomfort by mitigating post-concussion symptoms and may promote recovery by minimizing brain energy demands. However, there is currently insufficient evidence that complete rest achieves these objectives. A brief period of rest is still advised in the first 24-48 hours, but after this patients are encouraged to gradually and progressively increase their activity in a manner that does not worsen symptoms.
Closely monitored active rehab programs that involve controlled sub-symptom threshold, sub maximal exercise have been shown to be safe and beneficial in aiding recovery1.
Physiotherapy interventions have been found to be beneficial for the treatment of head or neck symptoms as well as vestibular symptoms. For vestibular symptoms like dizziness, vertigo, and poor balance, physiotherapy interventions can be used effectively to normalize an individual’s vestibular response. This type of rehab involves the use of specific exercises to alleviate symptoms of dizziness, as well as improve balance, eye coordination, and overall function4.
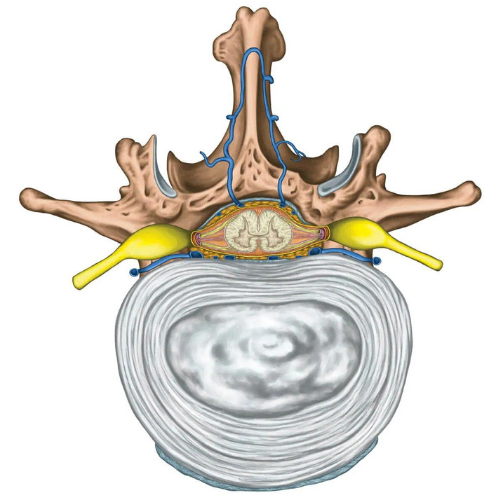
In athletes, neck strength has shown to have links to concussion risk. Increasing neck strength has the potential to decrease acceleration, deceleration, and change of direction forces experienced by the head. Greater neck strength was demonstrated to reduce the kinematic response of the head upon impact in adolescent soccer players as well as contact sport athletes5. A one pound increase of neck strength was associated with a 5% reduction in concussion risk6, therefore neck strengthening shows potential to decrease concussion risk, especially in adolescent athletes.
Return to activity decisions need to be made on an individualized basis. Current consensus research1 on concussions recommend the use of a graduated return to activity protocol that is outlined below:
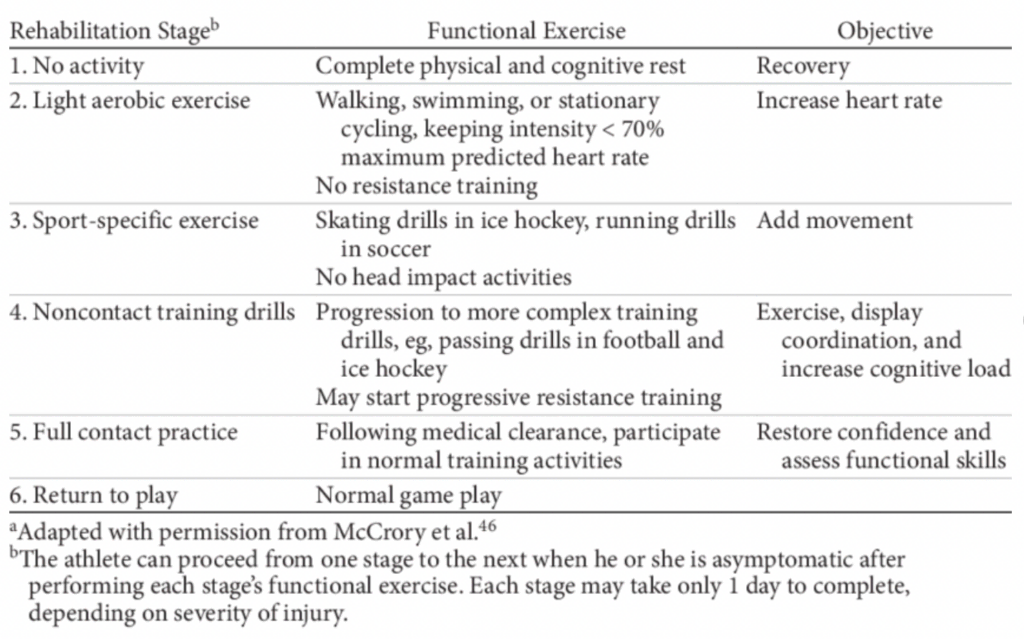
Using this protocol, you should gradually progress through each level before fully returning to activity. Progression to the next level requires you to remain symptom-free on the current level for 24 hours. If at any point during the protocol you have concussive symptoms, you must drop back to the previous symptom-free level. Progression can begin once more after a further 24-hour symptom-free period. Following the completion of this protocol, there should be no symptoms at rest or with exercise. Someone with a previous concussion should only be allowed to return to play when they are symptom-free AND not taking any medications that could alter their symptoms.
If you’re suffering from a concussion, contact us to book a consultation in our Toronto concussion clinic with one of our speciality trained healthcare providers.