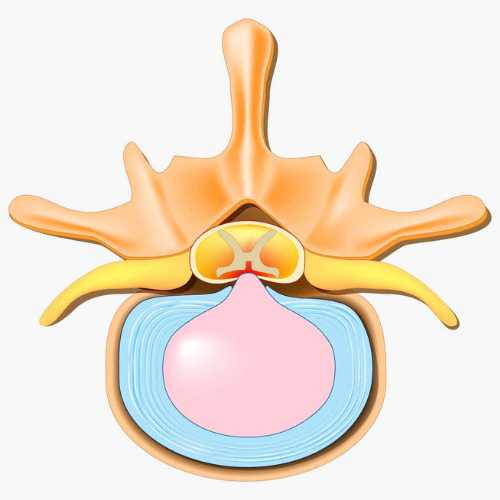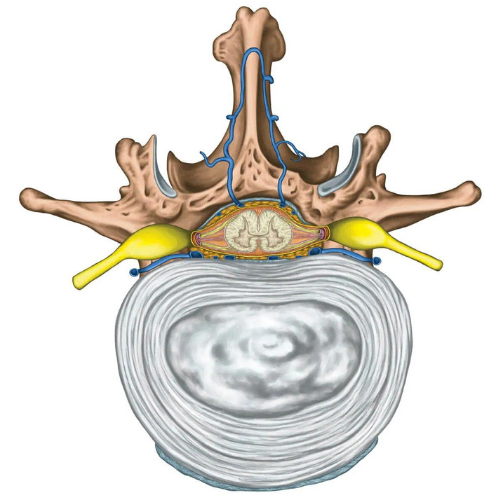
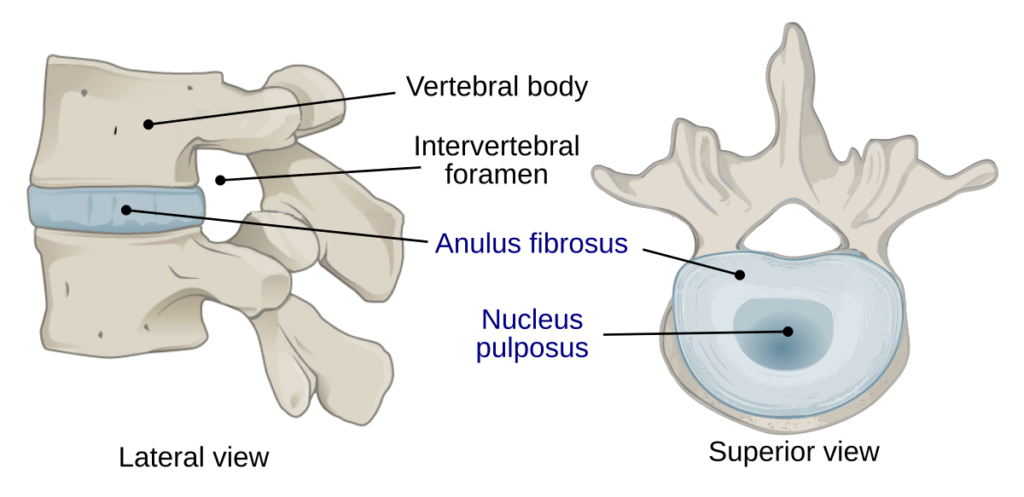
Degenerative disc disease (DDD) is an umbrella term for back pain or neck pain that results from or is associated with changes in the intervertebral discs1. Intervertebral discs form the joint between each vertebrae in your spine and allow for slight movement while acting as a ligament to hold the vertebrae together. These types of joints are extremely strong. The disc also plays a key role as as a shock absorber for your spine. Each disc has two parts:
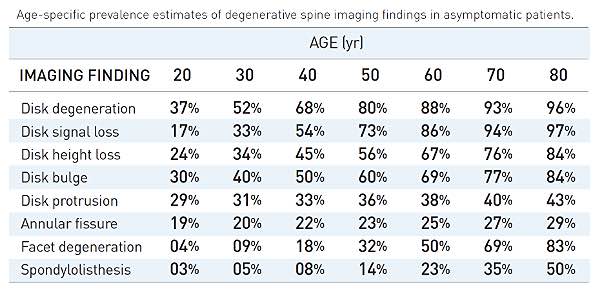
DDD can be present with or without symptoms, but is typically only identified when symptoms arise. Disc degeneration is considered a normal part of aging and often does not correlate with pain. Approximately 25% of people will show evidence of disc degeneration at one or more levels in the spine on MRI before the age of 40. Beyond age 40, this number goes up to 60% of people2.
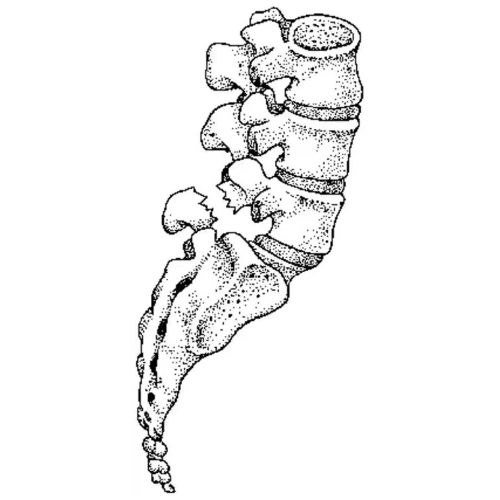
At birth, the nucleus pulposus contains about 80% water. Natural daily stresses and minor injuries can cause the annulus fibrosus to weaken over time and the disc to gradually lose water. The water loss results in a decrease in the size of the disc, which in turn decreases the space between vertebrae. As this space shrinks, more pressure is applied to the disc which may eventually cause tears in the annulus. If enough pressure is exerted, it is possible for the nucleus pulposus to leak out through these tears and cause a herniated disc. The loss of disc size also results in reduced ability to provide cushioning to the spine and as a result more force may be applied to the vertebrae. This can be a risk factor for arthritis, postural changes, stenosis, and inflammation and impingement of nerves associated with radiculopathy3. It is possible for DDD to develop at any level of the spine but is most common in the neck and lower back4.
Because DDD is largely the result of natural daily stresses and aging processes, it is not truly considered to be a disease process5.
The most common symptom of DDD is lower back pain or neck pain. The amount of degeneration of the disc does not have a strong correlation with pain. Whether or not you experience pain seems to largely depend on the location of the affected disc and how much pressure is applied to surrounding structures.
An affected disc in the lower back can typically present with lower back pain that may radiate to the hips, buttocks, thighs or legs. If pressure is being placed on nerves, it is possible to also experience sporadic tingling or weakness in the legs. An affected disc in the upper neck typically presents with pain in the neck, shoulders and arms. If nerves are affected, tingling or weakness in the hands and fingers may occur. These pains are most commonly experienced or aggravated by movements such as bending, lifting, and twisting or extended periods of sitting. Things that typically ease pain are staying active with frequent changes in position and lying flat on your back6.
DDD can often be successfully managed conservatively. Surgery may be recommended in cases that do not respond well to conservative management after a period of 3-6 months. Medications such as anti-inflammatory drugs are often used alongside conservative strategies in order to help manage symptoms while engaging in regular activities7.
Physiotherapy interventions typically involve load management strategies, regular physical activity, muscle strengthening and finding appropriate lifestyle adjustments.
Common approaches that have been have been found to be effective in pain reduction include movement facilitation exercises (McKenzie method) where a directional preference for movement is identified during assessment and repeated or sustained movements are used to reduce symptoms as well as core strengthening and core stabilization exercises8. Education to address fear-avoidance and empower patients to self-manage symptoms as they arise is a key component of long-term management of the condition9.