
What is spondylolysis?
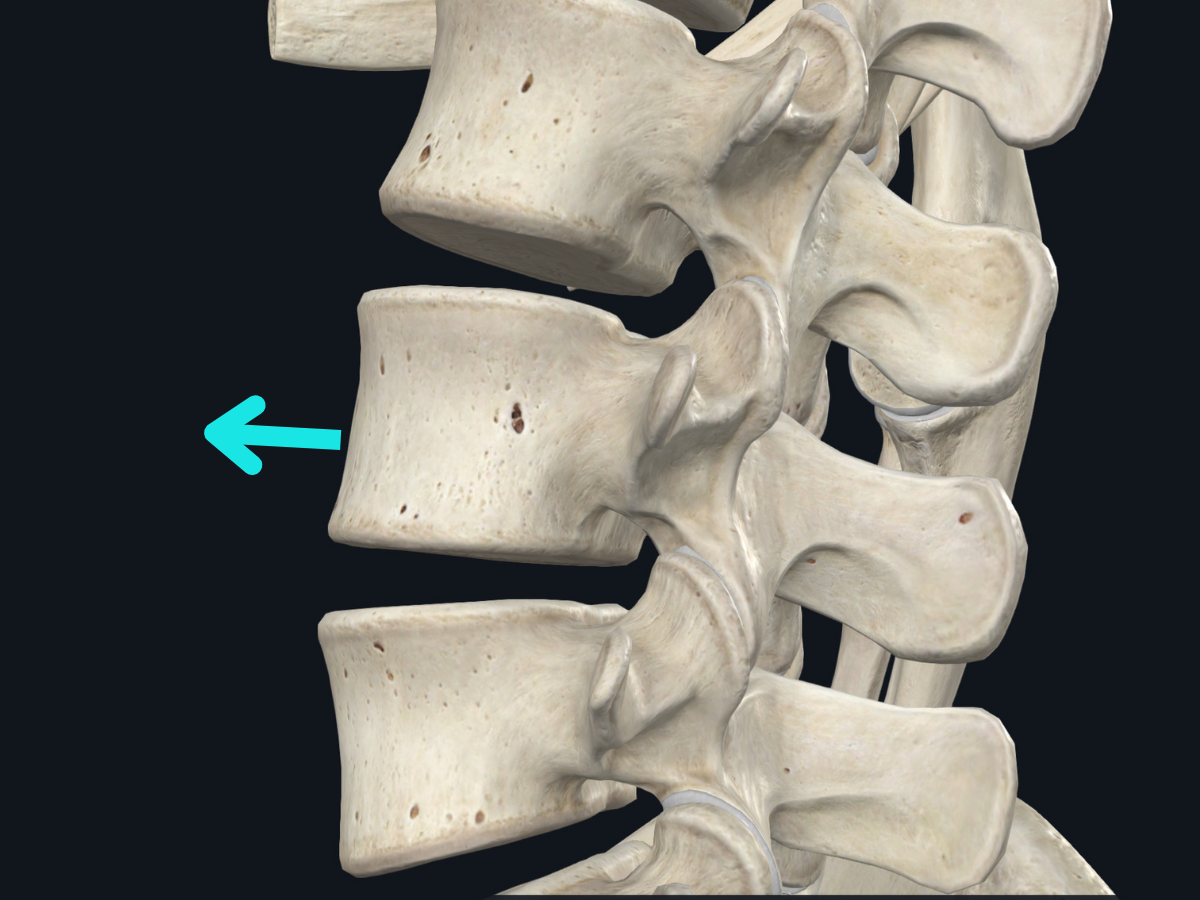
Spondylolysis, or a “spondy fracture”, is a condition that affects the bones in the spine. The bones in the spine are connected to each other by small joints called facet joints. These joints allow the spine to move and bend. The bones in the spine are also connected to the muscles and ligaments in the back. Spondylolysis occurs when there is a break in one of the bones in the spine. This break can occur in the facet joint or in the bone itself. The break usually occurs in the lower part of the spine (lumbar), near the tailbone.
What are the symptoms of spondylolysis?
The most common symptom of spondylolysis is lower back pain. The pain is usually worse with activity and improves with rest. Other symptoms may include:
- Stiffness in the lower back
- Muscle spasms in the lower back
- Difficulty bending or twisting the back (especially extension)
- Pain that radiates into the buttocks or legs
- Numbness or tingling in the legs
- Weakness in the legs

What are the symptoms of spondylolisthesis?
The most common symptom of spondylolisthesis is lower back pain. In some cases, the pain may radiate to the buttocks or legs. Other symptoms may include:
- Muscle tightness or spasms in the lower back
- Difficulty standing upright for long periods of time
- Difficulty walking or bending
- A feeling of instability in the lower back
- A grating or clicking sensation in the lower back
- Numbness or tingling in the legs or feet
What is the difference between spondylolysis and spondylolisthesis?
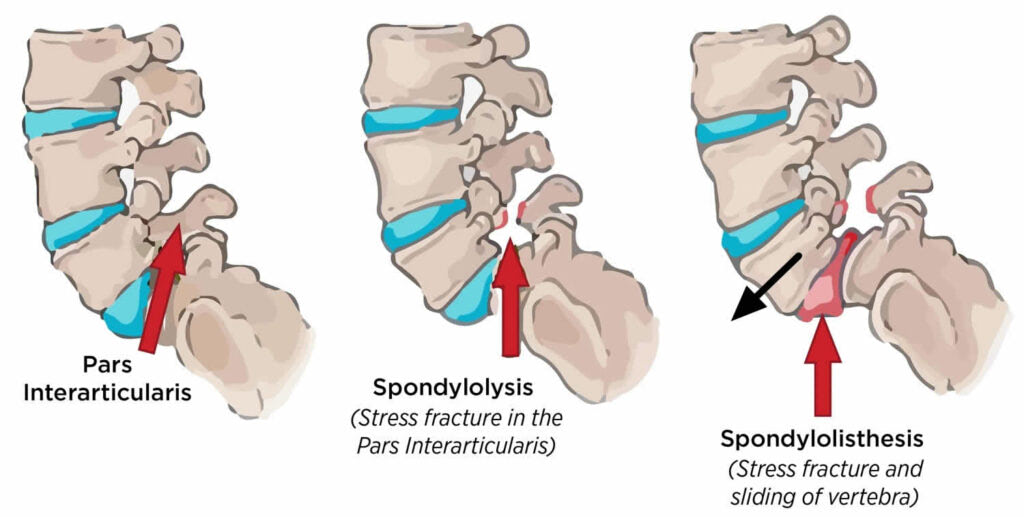
Spondylolysis is a condition that affects the vertebrae in the spine, causing them to become weak and susceptible to stress fractures. This can lead to a condition called spondylolisthesis, in which the vertebrae slip out of place and put pressure on the nerves in the spine.
What are the types of spondylolysis?
There are three types of spondylolysis: isthmic, dysplastic, and pars interarticularis.1 Isthmic spondylolysis is the most common type, and it occurs when there is a stress fracture in the pars interarticularis. Dysplastic spondylolysis is a congenital condition that results in a malformed pars interarticularis. Pars interarticularis spondylolysis is the least common type, and it occurs when the pars interarticularis is completely absent.
What are the types of spondylolisthesis?
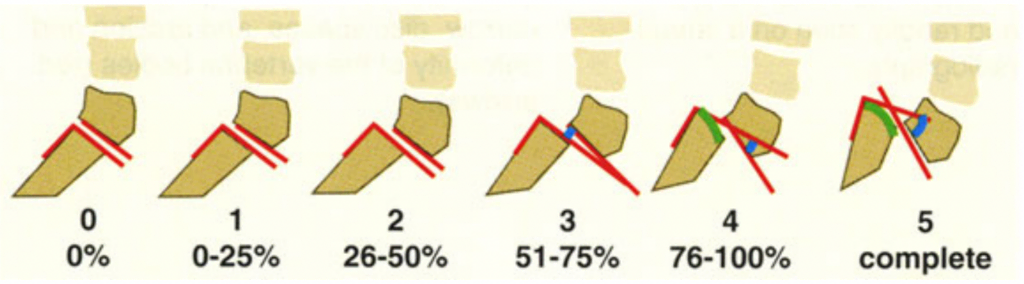
There are five types of spondylolisthesis, classified according to the causative mechanism:
- Type I: Congenital
- Type II: Iatrogenic
- Type III: Traumatic
- Type IV: Pathologic
- Type V: Degenerative
There are also five grades of spondylolisthesis, with grade I being the least severe and grade V being the most severe.
How common is spondylolysis and spondylolisthesis?
Spondylolysis is a relatively common condition, occurring in about 4-6% of the population.1 However, only a small percentage of people with spondylolysis will go on to develop spondylolisthesis.
Spondylolysis is most common in people who play sports that involve a lot of back and leg movement, such as gymnastics, football, and wrestling. It is also more common in people who have family members with the condition.
The prevalence of spondylolisthesis is difficult to determine because it is often asymptomatic and undiagnosed. Estimates range from 0.5% to 7% of the population.1 Spondylolisthesis is very common in children and adolescents, but rare in adults after skeletal maturation.
How is a pars fracture diagnosed on imaging?
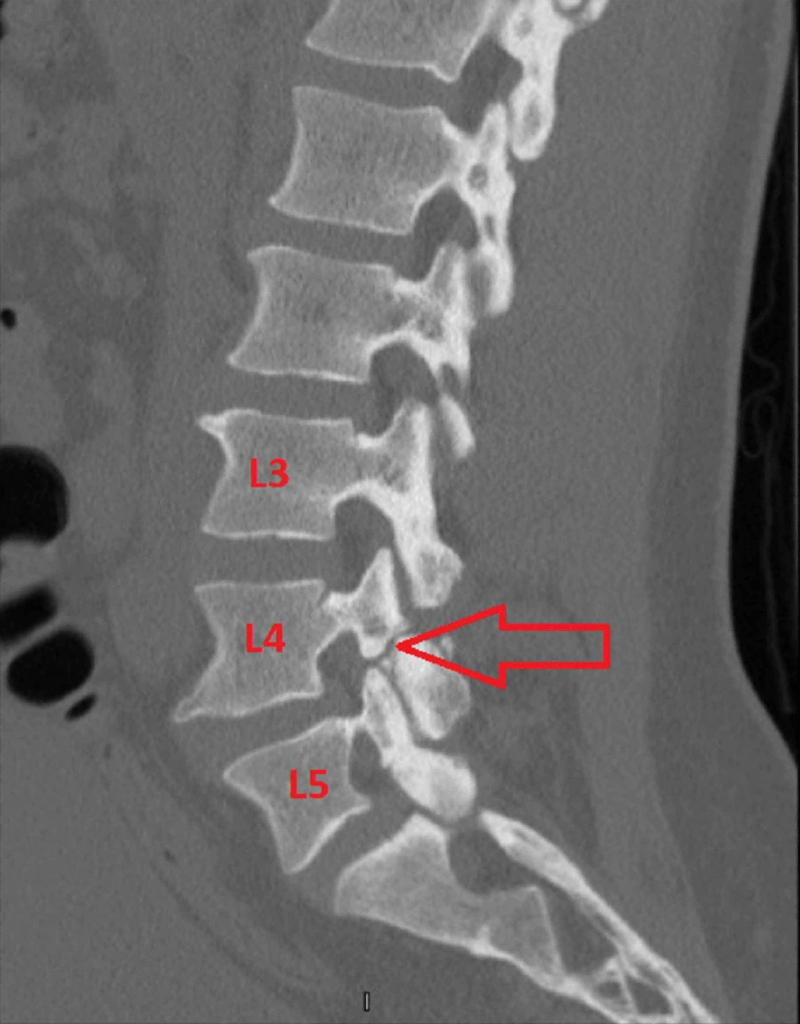
It is difficult to diagnose in the early stages using regular x-rays, but there are two hallmark findings that can be seen on MRI and CT scan that can help with diagnosis: bone marrow edema of the adjoining pedicle on MRI and bone absorption at the caudal aspect on the sagittal reconstructed CT scan.
What is the treatment for spondylolysis?
There are two goals for treating pars fractures: healing the bone (in the early and progressive stages) and managing pain (in the terminal stage). In the early and progressive stages, bone healing is encouraged with the use of a hard lumbar brace, however, the need for a lumbar brace is still debated.
In the terminal stage, we focus on managing pain because there is low to no possibility of healing the bone. A lumbosacral soft brace can be used to prevent extension movements of the spine. When pain persists, steroid injections in the defects and use of NSAIDs are other options. Almost all patients can return to the baseline activity with conservative management.
Spondylolysis is a disorder that usually goes away on its own or with conservative treatment, but in some cases surgery is needed. Two surgeries - the Buck or Scott procedure - seem to help.2 The first surgery is used more often and is when a screw is placed in the back to help compress or hold things together. The second surgery, the Scott procedure, is when wires are used to try and hold things together. There is evidence that these procedures work better in people who are under 25 years old. After surgery, athletes can usually return to sports within 6-12 months.
Rehabilitation for spondylolysis
Athletes with spondylolysis should avoid extension and rotation motions when they are first injured, but should gradually start doing these motions again as they get better. Clinicians should also remember that although there is a bone stress injury in the lumbar spine, athletes use their entire body when participating in sports. Impairments in other regions can increase stress throughout the lumbar spine and should be addressed.
The first phase of the program is performed in a relatively static and neutral lumbar position allowing for muscle activation and strengthening while avoiding undue stress on the injured pars interarticularis. The deep abdominals and lumbar multifidus are addressed.
In phase two, as the patient's symptoms improve, extension and rotation motions are reintroduced with the goal of returning to sport.3
Is a back brace needed for low back pain?

There is some controversy about whether lumbar bracing is effective in treating spondylolysis. Some people think it is helpful, but a recent study found that it might not be any better than not wearing a brace. More research is needed to figure out if lumbar bracing is effective, however we’ve summarized a few recent studies below that have successfully used lumbar bracing.
Athletes who have spondylolysis are often treated with a thoracolumbosacral orthosis (TLSO), which is a brace that goes from the chest to the hips and is worn under the clothes. Some athletes wear a lumbosacral orthosis (LSO), which is a brace that goes from the waist to the upper thigh.
Different conservative regimens have been described, most commonly involving use of the TLSO brace. Micheli et al treated 12 athletes with spondylolysis using a TLSO brace and achieved good or excellent results with a treatment duration of 4 to 24 months. Sys et al reported treating 28 athletes with a TLSO brace for an average treatment period of 4 months; 89.3% of these athletes returned to previous levels of competitive activities in an average of 5.5 months.2
There is no gold standard approach for the management of spondylolysis in the athletic population, but the existing literature indicates that athletes with spondylolysis can benefit from conservative management in the form of a TLSO or LSO brace for 3-6 months complemented by activity modification and physiotherapy.4
Should I continue playing sports with a spondy fracture?
People with spondylolysis should stop playing sports for at least three months, and physiotherapy should be started early (within a few weeks) after the diagnosis, to reduce muscle atrophy, deconditioning, and potentially reduce time out of sport.
References
- https://link.springer.com/book/10.1007/978-3-030-26207-5
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4993622/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7134351/
- https://www.sciencedirect.com/science/article/pii/S1529943022001681


.png)
