What is plantar fasciitis?
Plantar fasciitis, also known as plantar fasciopathy or plantar heel pain, is one of the most common causes of foot pain. It is an irritation of the plantar fascia and the surrounding structures. It is estimated that 1 in 10 people will experience it in their lifetime, with 2 million people receiving treatment for it every year.1
What is the plantar fascia?
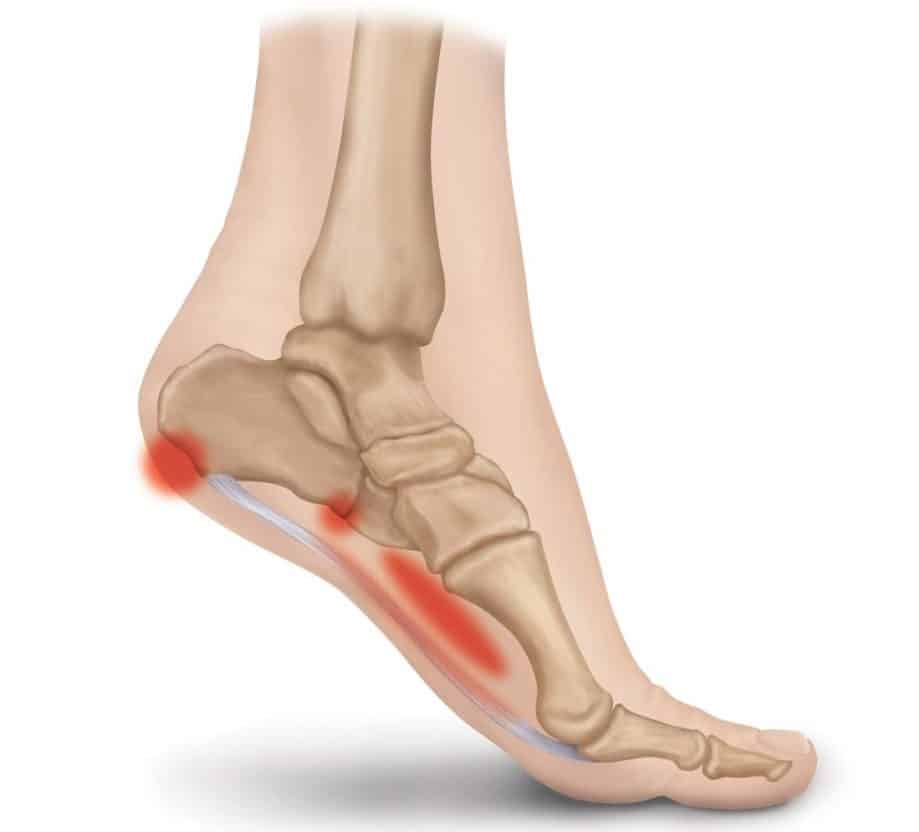
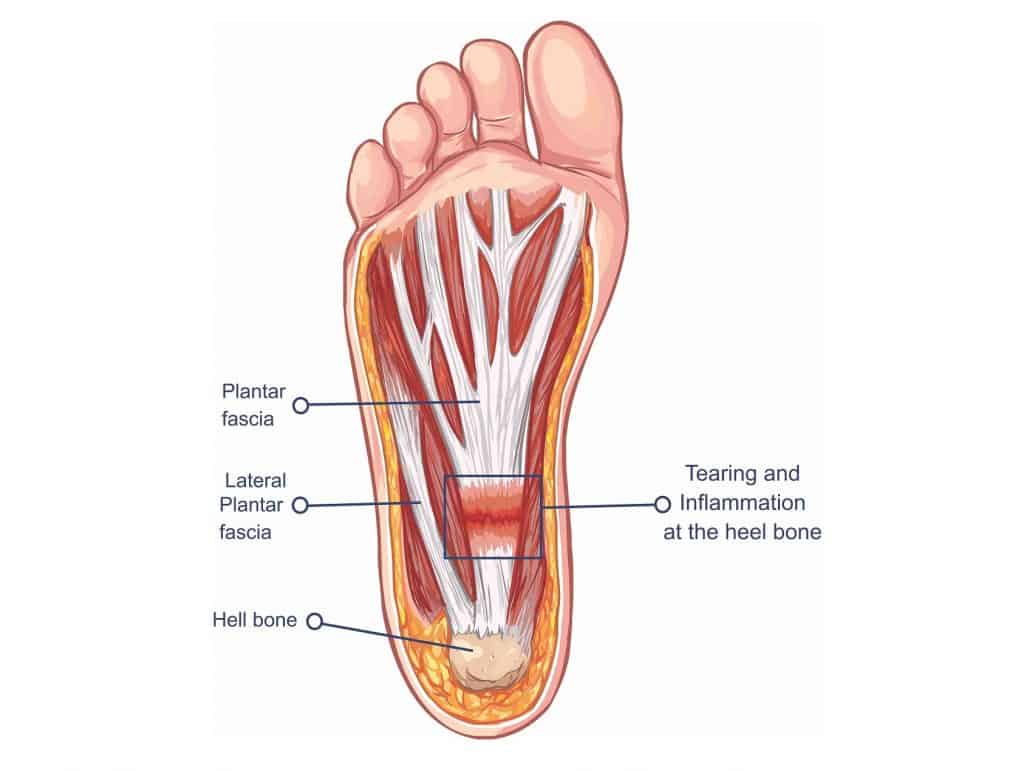
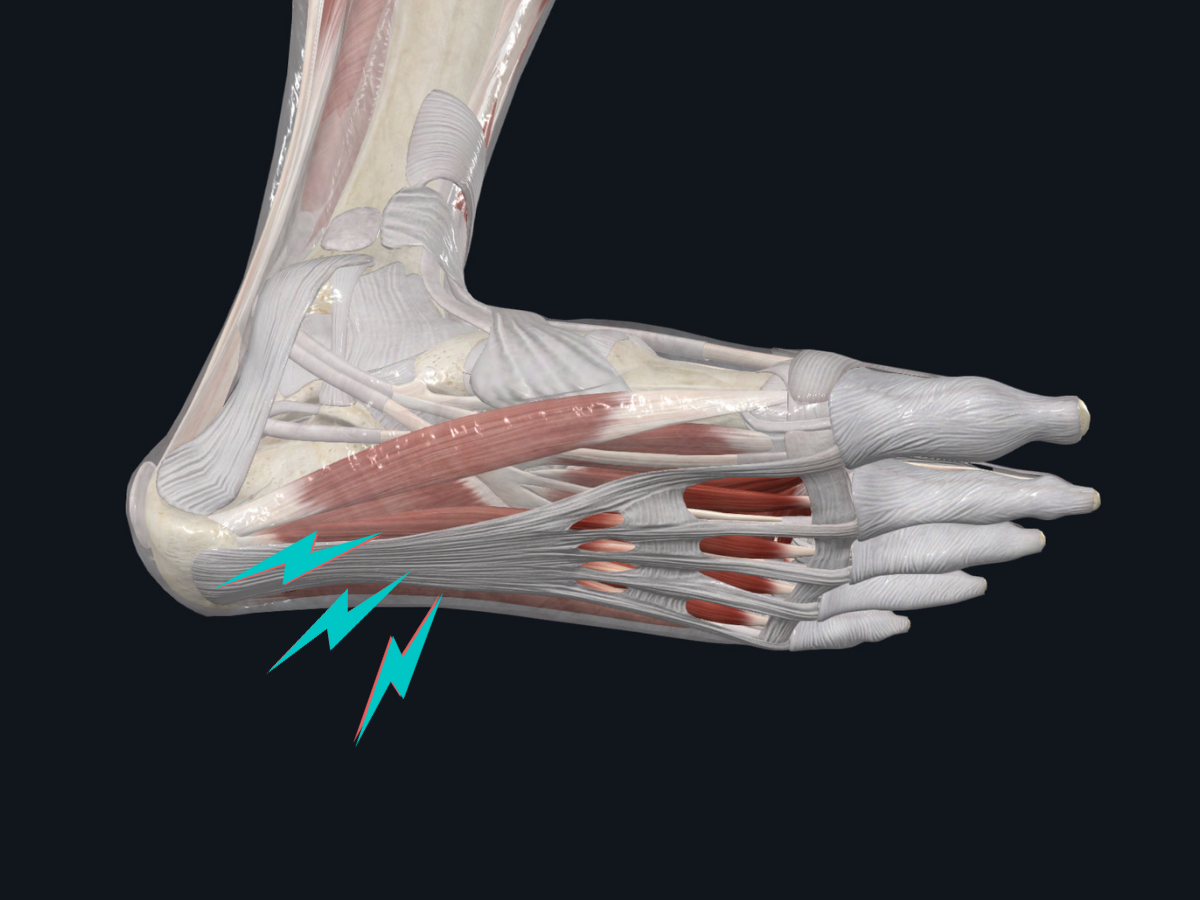
The plantar fascia is a thick band of connective tissue that supports the arch of the foot. It attaches to the medial side of the heel bone and then divides into five bands inserting at the base of each toe and the metatarsal heads. The tensioning of the plantar fascia during weight bearing activities allows for added stability in a loaded foot with minimal muscle activity.2 The plantar fascia also plays a dynamic role during walking where it stretches, stores potential energy, provides a rigid structure for propulsion, then passively contracts, converting the previously stored potential energy into kinetic energy and aiding acceleration.3
What are the symptoms of plantar heel pain?
Patients typically complain of sharp pain along the inside of the heel when walking in the morning and after a period of rest that gets better after walking for a period of time. It usually worsens at the end of the day and with impact sports and activities.4
What causes plantar fasciitis?
While the causes of plantar heel pain are multifactorial it is primarily due to overload and repetitive microtrauma. This results when the total load the foot is exposed to has changed or increased faster than the plantar fascia has been able to adapt. This is often due to an increase in weightbearing activities, but it can also be the result of a change in training surface, footwear, or a combination of factors including distance, intensity and volume.
Risk factors include obesity, prolonged weight-bearing, altered biomechanics with poor ankle mobility, calf and Achilles tendon tightness, weak intrinsic muscles of the feet, excessive foot pronation, and poor footwear.5
What is the best treatment for plantar fasciitis?
The first-line choice for plantar heel pain is conservative management, such as physiotherapy or chiropractic. It has been shown that 82% of patients responded favorably to conservative therapy6 and the proportion of patients requiring surgery is less than 2%.7 A program of calf-stretching and eccentric loading has been confirmed to be an effective treatment.8 Treatment typically includes relative rest from aggravating activities combined with stretches targeting the plantar fascia, Achilles tendon, and calf muscles.2 High load strength training is effective in the mid-late stage treatment of plantar heel pain and has been shown to aid in pain reduction, improvement of function, and prevention of injury reoccurrence.9
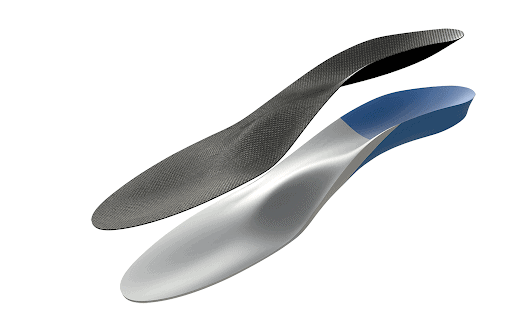
Should I get orthotics for plantar fasciitis?
Orthotics have been shown to produce some small reductions in pain for people with plantar heel pain.10 When used in conjunction with a stretching and strengthening program, a custom orthotic and even an appropriate shoe insert are likely to produce improvements in symptoms as part of the initial treatment phase.11
Should I get a cortisone injection for plantar heel pain?
Steroid injections are often effective at reducing symptoms in the short term, however, the positive effects usually last no longer than one month. Additionally, multiple injections may increase the risk of rupture of the plantar fascia as well as fat pad atrophy.12 Due to the limited benefits and potential complications, steroid injections should only be used in cases where symptoms are not settling with conservative management.
Conclusions
- Plantar heel pain is a common condition and is prevalent in both athletic and non-athletic populations.
- It is self-limiting and responds to conservative treatment in almost 90% of patients.
- Altered biomechanics are believed to contribute to the condition through decreased ankle joint range of motion
- The use of eccentric calf stretching with additional exercises for the surrounding structures is currently the treatment of choice for chronic plantar heel pain.
References
- Volume of ambulatory care visits and patterns of care for patients diagnosed with plantar fasciitis: a national study of medical doctors. Riddle DL, Schappert SM Foot Ankle Int. 2004 May; 5(5):303-10
- Cheung JT-M, An K-N, Zhang M. Consequences of partial and total plantar fascia release: a finite element study. Foot ankle Int / Am Orthop Foot Ankle Soc [and] Swiss Foot Ankle Soc. 2006;27(2):125–32
- Cutts S, Obi N, Pasapula C, Chan W. Plantar fasciitis. Ann R Coll Surg Engl. 2012;94(8):539-542. doi:10.1308/003588412X13171221592456
- Barouk LS, Baudet B, Bonnel F, et al. Gastrocnemius tightness: from anatomy to treatment. Montpellier: Sauramps Médical, 2012.
- Plantar fasciopathy: revisiting the risk factors. Beeson P Foot Ankle Surg. 2014 Sep; 20(3):160-5.
- The management of subcalcaneal pain.Snook GA, Chrisman OD Clin Orthop Relat Res. 1972 Jan-Feb; 82():163-8.
- Plantar fasciitis. The painful heel syndrome. Furey JG J Bone Joint Surg Am. 1975 Jul; 57(5):672-3.
- Tissue-specific plantar fascia-stretching exercise enhances outcomes in patients with chronic heel pain. A prospective, randomized study. DiGiovanni BF, Nawoczenski DA, Lintal ME, Moore EA, Murray JC, Wilding GE, Baumhauer JF J Bone Joint Surg Am. 2003 Jul; 85(7):1270-7
- Rathleff, M.S., Mølgaard, C.M., Fredberg, U., Kaalund, S., Andersen, K.B., Jensen, T.T., Aaskov, S. and Olesen, J.L., 2015. High‐load strength training improves outcome in patients with plantar fasciitis: A randomized controlled trial with 12‐month follow‐up. Scandinavian journal of medicine & science in sports, 25(3)
- Landorf KB, Keenan AM, Herbert RD. Effectiveness of foot orthoses to treat plantar fasciitis: a randomized trial. Arch Intern Med. 2006 Jun 26;166(12):1305-10. (level of evidence: 1b)
- Pfeffer G, Bacchetti P, Deland J et al. Comparison of custom and prefabricated orthoses in the initial treatment of proximal plantar fasciitis. Foot Ankle Int. 1999 Apr;20(4):214-21. (level of evidence: 2b)
- Injected corticosteroids for treating plantar heel pain in adults. David JA, Sankarapandian V, Christopher PR, Chatterjee A, Macaden AS Cochrane Database Syst Rev. 2017 Jun 11; 6():CD009348.

.png)
