What is a torn biceps tendon?
A distal biceps rupture is a tear in the tendon that connects the biceps muscle to the forearm. This type of injury is relatively rare, occurring in 1.2 to 2.55 out of every 100,000 people each year.1 The incidence of distal biceps rupture is higher in young, active people participating in contact sports, and in middle-aged men from fourth to sixth decades. A torn biceps tendon is more likely to happen on the dominant arm.
What are the risk factors for a biceps rupture?
Risk factors for a distal biceps rupture include:
- smoking
- steroid use
- obesity
- history of similar injuries, or tendinopathy
- People who push or lift heavy objects
- Chronic renal disease
What are biceps tendon rupture symptoms?
A prodromal symptom is a symptom that happens before the main symptom. In the case of a biceps tear, the prodromal symptom would be an aching sensation in the elbow. 10% of patients with a full thickness distal biceps rupture report a painful "pop" sensation. Anterior elbow pain, anterior arm and elbow swelling, and weakness of elbow flexion and forearm supination are commonly reported symptoms. Tasks such as turning a key, using a screwdriver and opening a jar are difficult to do.

In a torn distal biceps, there would be bruising, swelling, and a prominent biceps bulge at the anterior mid-arm level (what is known as the Popeye sign). If you feel the area where the biceps muscle is, it would be tender and there would be a defect in the case of a complete tear. The amount of proximal retraction (i.e. where the biceps rolls back towards the shoulder) would depend on the partial or complete rupture of the distal biceps and the integrity of structure called the lacertus fibrosus. The lacertus fibrosus is a fascial thickening that connects the distal biceps to the forearm flexor muscles and provides stability to the distal biceps tendon. It also helps prevents retraction of the torn distal biceps tendon.
How is a rupture of the biceps tendon diagnosed?
The Hook test is a test used to diagnose acute, complete ruptures and to evaluate postoperative recovery of the distal biceps tendon. The test is done by hooking the tendon with the examiner's finger inserted from the outer side of the tendon. Repeating the same manoeuvre from the inner side would give information about the anatomical integrity of the lacertus fibrosus.
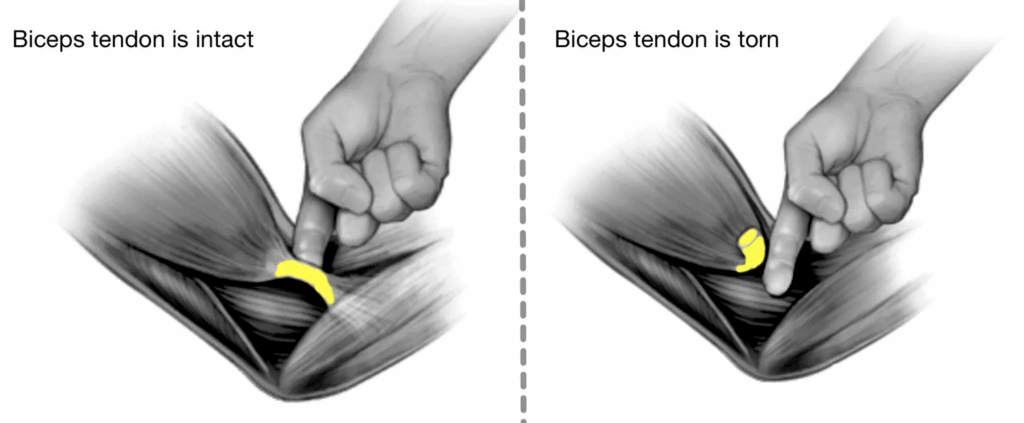
Another test is called the Biceps Squeeze test. The Biceps squeeze test is used to figure out if someone has a completely torn biceps tendon. To do the test, the person sits with their elbow at a 70-90 degree angle and their arms by their sides. The examiner then squeezes the bulky part of the biceps muscle. If the distal biceps tendon is intact, the forearm should start to move into a pronated position. If the forearm does not move, it is likely that the biceps tendon is completely torn.
What medical imaging should be done to detect a torn distal biceps tendon?
In order to rule out any bony injuries, such as a coronoid fracture, that could be causing pain in the elbow, an X-ray would be taken. If the X-ray showed no bony injuries, then an MRI would be considered the gold standard for diagnosing distal biceps pathologies. The MRI can show any partial tears, and measure the extent of tendon retraction in acute or chronic tears. Diagnostic ultrasound is a less expensive but still reliable investigation for diagnosing various pathologies of the distal biceps.
Is surgery needed for a ruptured biceps tendon?
If the biceps tendon is completely torn, and the lacertus fibrosus (a nearby structure) is also torn, then the biceps tendon can retract significantly and might not be able to be repaired. However, if the lacertus fibrosus is intact, and there is no significant retraction of the biceps tendon, then primary repair (surgery to fix the tendon) may still be possible. If the biceps tendon is completely torn and is not repaired, it can cause problems later on.
If you have a partial rupture of your biceps tendon, your doctor may recommend non-operative treatment, which means you won't have surgery. If your rupture is more than 50% of the tendon thickness, or if you have failed non-operative treatment for a partial rupture, you may need surgery.1 This surgery involves debridement, or removal of damaged tissue, and fixation of the biceps tendon.
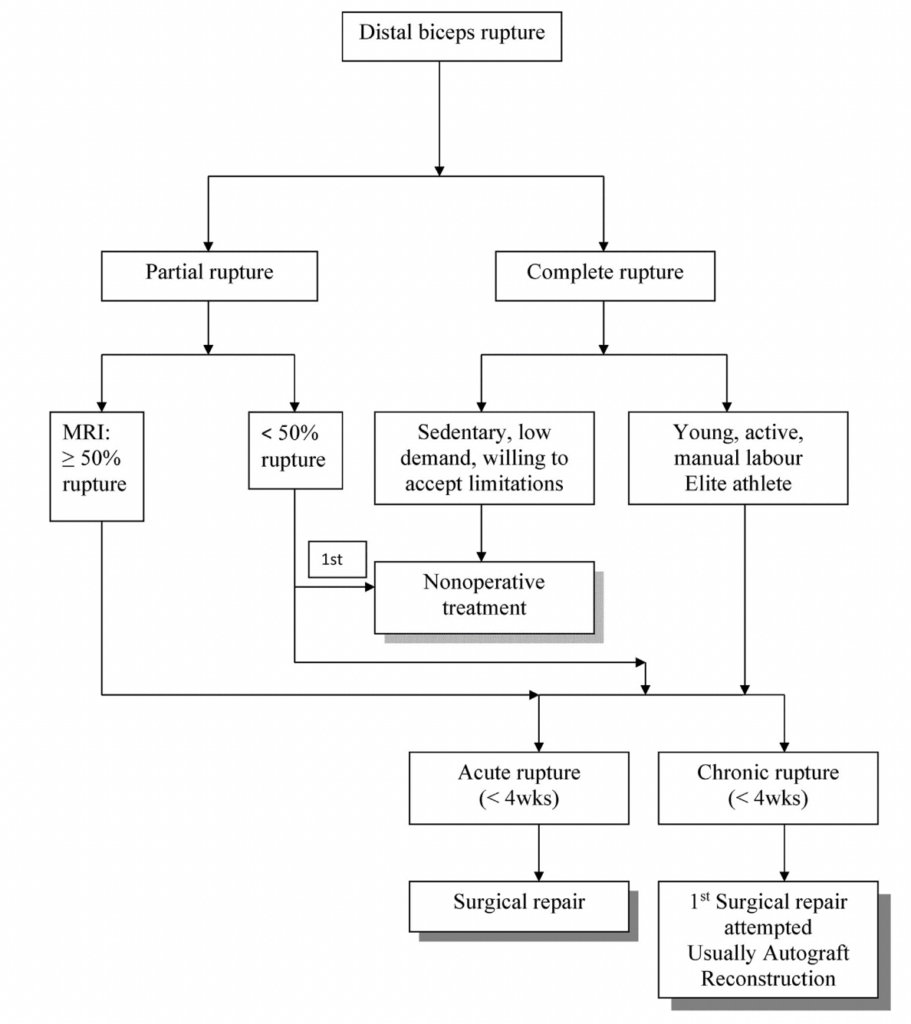
Surgery is recommended for young patients who have a recent, complete tear in their tendon. The surgery aims to fix the torn tendon to the bone so that it can heal properly. There are two ways to do this surgery-- single incision or double incision. Single incision is easier to perform but may not heal the tendon as well as double incision. Double incision involves making two cuts, one from the front and one from the back, in order to reach the tendon and fix it in place. After the surgery, patients are usually able to return to work within 3-4 months.
Non-operative treatment is recommended for patients who are unwilling or unable to have surgery. This means that they should be told about the possible downside of not having the tendon repaired, which could lead to not being able to use the hand as well as before. However, sometimes surgery is not possible because the tendon has been ruptured for a long time and has shrunk and become scarred to the surrounding tissues. If surgery is attempted, it may not be possible to fix the tendon in its original place and additional procedures may be needed. These could include using a tendon from another part of the body or from a donor. There is still disagreement among doctors about which of these methods works better.
Is biceps tendon re-rupture common?
Rerupture after distal biceps tendon repair is not common, happening to 1-5% of people who have the surgery.2 Most of the time, it happens because the person doesn't follow the recommended post-op instructions or has an accident. Smoking also makes it more likely to happen. There is no difference in the rates of rerupture between people who have single-incision or two-incision surgery.
What is the recovery time for a torn biceps?
Recovery and rehabilitation after surgical repair of a torn biceps tendon takes approximately 6 months, and longer with individuals returning to a competitive sport that involves the injured arm. In some cases, with poor or delayed treatment, functional deficits can persist for years. That is why it is important to fully complete your care plan in order to maximize your recovery.
What is the rehabilitation process after biceps tendon repair surgery?
Patients who have surgery to repair the tear tend to have better outcomes than those who don't have surgery, however there is no consensus on the best way to rehabilitate this injury.2
Phase 1
The postoperative rehabilitation program for people who have had surgery to repair their distal biceps follows a multi-phased, criteria-based progression designed to help them return to their previous level of activity and function as quickly and safely as possible. The first phase of the rehabilitation process is designed to promote healing of the surgical repair, reduce pain and inflammation, and regain full motion of the wrist, hand, and shoulder. During this phase, the patient's elbow is immobilized in a splint and they are instructed to use cryotherapy 6-8 times per day. The patient is also started on exercises to reduce muscular atrophy and stretching exercises to avoid stiffness.
Phase 2
The second phase of rehabilitation after elbow surgery typically begins at the start of postoperative week 2 and ends after week 6. This phase of the rehabilitation process focuses on the gradual restoration of elbow ROM, improving muscular strength and endurance, and introducing cardiovascular fitness training.
Phase 3
The third phase of the rehabilitation process typically begins 7 weeks after surgery and emphasizes the full restoration of elbow range of motion. Exercises during this phase also focus on maintaining upper body mobility, improving muscular strength and endurance at the wrist and shoulder, and adding isometric biceps-strengthening exercises. It is important to progress elbow extension activities from a supinated forearm position to a neutral position and finally to a pronated forearm position to slowly increase the amount of stretch on the distal biceps repair. Manual ROM/stretching and mobilization techniques can become more aggressive toward weeks 8–10 after surgery, but healing constraints of the involved tissue, the surgical technique performed, and the end feel of the motion being assessed must be taken into account. Improving the flexibility of the upper body, except the biceps, should now become a focus and include maintaining optimal shoulder flexibility, particularly in individuals who would like to return to overhead athletic activities.
Overhead athletes need to have a normal range of motion in their shoulders. Patients should start doing isotonic exercises, which are exercises with resistance, at 8 weeks. They should use weights that increase by ~1 pound each week. They should also start doing isometric exercises, which are exercises without resistance, at 8 or 10 weeks. Neuromuscular control exercises are introduced and progressed to help the shoulder and elbow muscles better work together.
Phase 4
The fourth phase starts at the beginning of week 12 and continues through week 16. The focus of this phase is maintaining (or restoring) elbow and upper extremity mobility. The patient should also start doing light biceps strengthening exercises between weeks 10 and 12, gradually increasing the weight being lifted. The focus should be on eccentric biceps strengthening by the end of this phase. Upper and lower extremity strengthening should also be increased during this phase. A progressive return to throwing can begin at around 12-14 weeks.
Phase 5
The advanced strengthening phase is the fifth phase of rehabilitation for a biceps tendon tear. This phase starts at week 16 and continues through week 20. The goals of this phase are to increase muscular strength and endurance in the surgically repaired biceps while increasing upper extremity power and neuromuscular control. This phase also introduces plyometric exercises, which are important to develop muscular power in the upper extremity.
Phase 6
The final phase, return to activity, allows the patient to go back to all the activities they did before the surgery. This includes things like sports and recreation. The exercises in this phase are based on what the patient wants to achieve. Before beginning this phase, the patient's strength and movement in the elbow and wrist should be at least 90% of the strength in the uninvolved arm.
References
- Vishwanathan, K., & Soni, K. (2021). Distal biceps rupture: Evaluation and management. Journal of Clinical Orthopaedics and Trauma, 19, 132–138. doi:10.1016/j.jcot.2021.05.012
- The Management of Biceps Pathology: A Clinical Guide from the Shoulder to the Elbow – Jan. 26 2021 ; ISBN-13. 978-3030630188


.png)
