In the summer of 2023, I developed costochondritis. Costochondritis is a common cause of chest pain, which can be alarming for many people. However, it’s important to know that this condition is often benign and unrelated to heart problems. I've had a few injuries in my life, and despite this condition not being considered serious, it still ranks as the most painful and scary.
Before I share my story, let's break down what costochondritis is, what causes it, and how it’s treated, based on expert-reviewed medical literature.
What is Costochondritis?

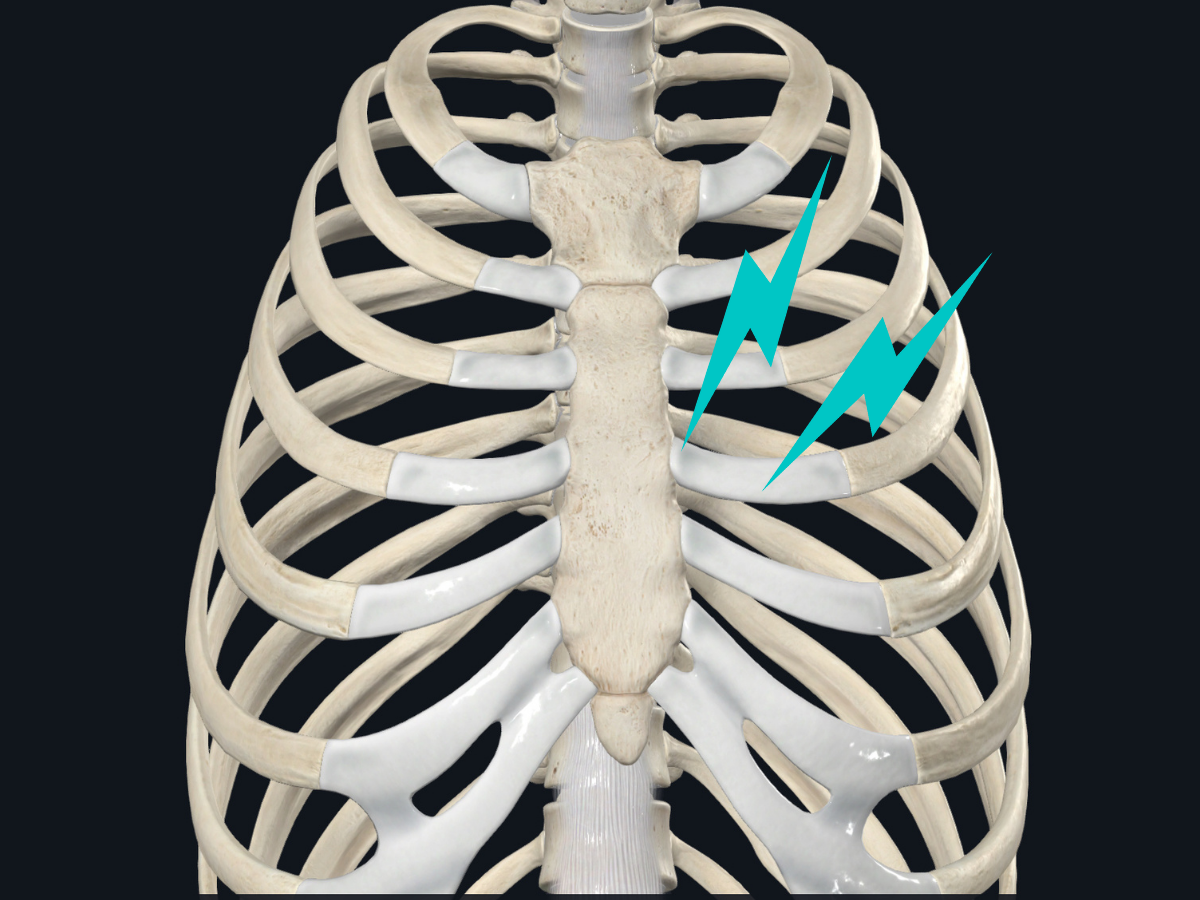
Costochondritis is a condition characterized by inflammation in the cartilage that connects the ribs to the breastbone (sternum). This area is called the costochondral joint. When this joint becomes inflamed, it causes pain in the chest wall, which can be confused with more serious heart-related chest pain.
While it can happen at any age, costochondritis is most common in adults aged 40 to 50. Women seem to be slightly more affected than men.
What Does Costochondritis Feel Like?
People with costochondritis typically experience chest pain that:
- Is sharp and aching.
- Gets worse when you take deep breaths, cough, or stretch.
- Tends to be located on both sides of the chest, especially where the ribs connect to the breastbone.
- May be tender to the touch but doesn’t usually come with swelling, redness, or warmth in the area.
This pain can sometimes feel scary because chest pain is often associated with heart attacks. However, costochondritis pain doesn’t involve other classic heart attack symptoms like radiating pain in the arms or shortness of breath.
What Causes Costochondritis?
It's unknown what causes the inflammation that leads to costochondritis, but some common triggers include:
- Physical strain or injury: Heavy lifting, strenuous exercise, or trauma to the chest can sometimes lead to costochondritis.
- Infections: Though rare, bacterial or fungal infections can affect the cartilage in the ribs, especially after surgery.
- Arthritis or joint inflammation: Some people with inflammatory conditions like arthritis may develop costochondritis.
Interestingly, costochondritis is also seen more frequently in adolescents and young adults who are active or who experience musculoskeletal pain in their chest.
My episode started after resuming my exercise routine after a period of inactivity. I felt a tightness across my chest after doing a few sets of bench presses.
How Is Costochondritis Diagnosed?
There’s no single test to diagnose costochondritis. Instead, doctors rely on a thorough history and physical exam. The most telling sign is pain that can be reproduced by pressing on the costochondral joints. Other physical maneuvers, like the crowing rooster or crossed-chest adduction maneuvers, can also help confirm the diagnosis.
It’s important to rule out more serious causes of chest pain first, such as heart problems, lung issues, or gastrointestinal conditions, especially if the person has risk factors like a history of heart disease.
My Experience
When the chest pain first started, I was understandably very concerned. The sharp, aching discomfort was so intense one night that it prevented me from lying down. I decided to go to the emergency room to get it checked out. The ER doctors took my symptoms very seriously and immediately began a thorough evaluation to rule out a heart attack or other serious underlying condition.
The ER team ordered several additional tests. They ran an electrocardiogram (ECG) to check the electrical activity of my heart and assess for any signs of a heart attack or other cardiovascular problems. They also took chest X-rays to look for any abnormalities in my ribs or chest wall. Additionally, they drew blood to check for other important markers to aid in diagnosis.
Thankfully, all of the test results came back normal, which helped rule out more serious conditions and point the doctors towards a diagnosis of costochondritis. They explained that while the chest pain I was experiencing was quite severe, it was likely caused by the inflammation in the cartilage connecting my ribs to the breastbone - a benign musculoskeletal issue rather than a life-threatening cardiac event.
Even though the ER visit was stressful, I was relieved to learn that my symptoms were not indicative of a heart attack or other major health problems. As a physiotherapist, I knew that costochondritis, while painful, is usually a self-limiting condition that responds well to conservative treatment.
Treatment: What Can Be Done About It?
Fortunately, costochondritis usually goes away on its own with time and simple treatments. The main goal is to manage the pain and inflammation until the condition resolves. Here are the most common treatments:
- Rest and Avoiding Strain: Taking a break from activities that worsen the pain is often recommended. This gives the inflamed area time to heal.
- Applying Heat: Many patients find relief from using heat pads on painful areas, although this hasn’t been studied in clinical trials.
- Medications: Nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen are often prescribed to reduce pain and inflammation. However, there’s no strong scientific evidence supporting their effectiveness for this specific condition. In my experience treating similar cases, NSAIDs don't seem to help, but it's an easy remedy to try.
- Topical Treatments: Creams or patches containing capsaicin, lidocaine, or diclofenac can be applied directly to the painful area. These are commonly used in treating other inflammatory conditions and may provide relief for costochondritis too.
- Physiotherapy: A targeted stretching program under the supervision of a physiotherapist or Chiropractor can help alleviate pain, especially if symptoms last for more than a year.
- Injections: In cases where symptoms persist and do not respond to other treatments, corticosteroid injections into the affected area may help. However, this is typically a last resort and should only be done under medical supervision.
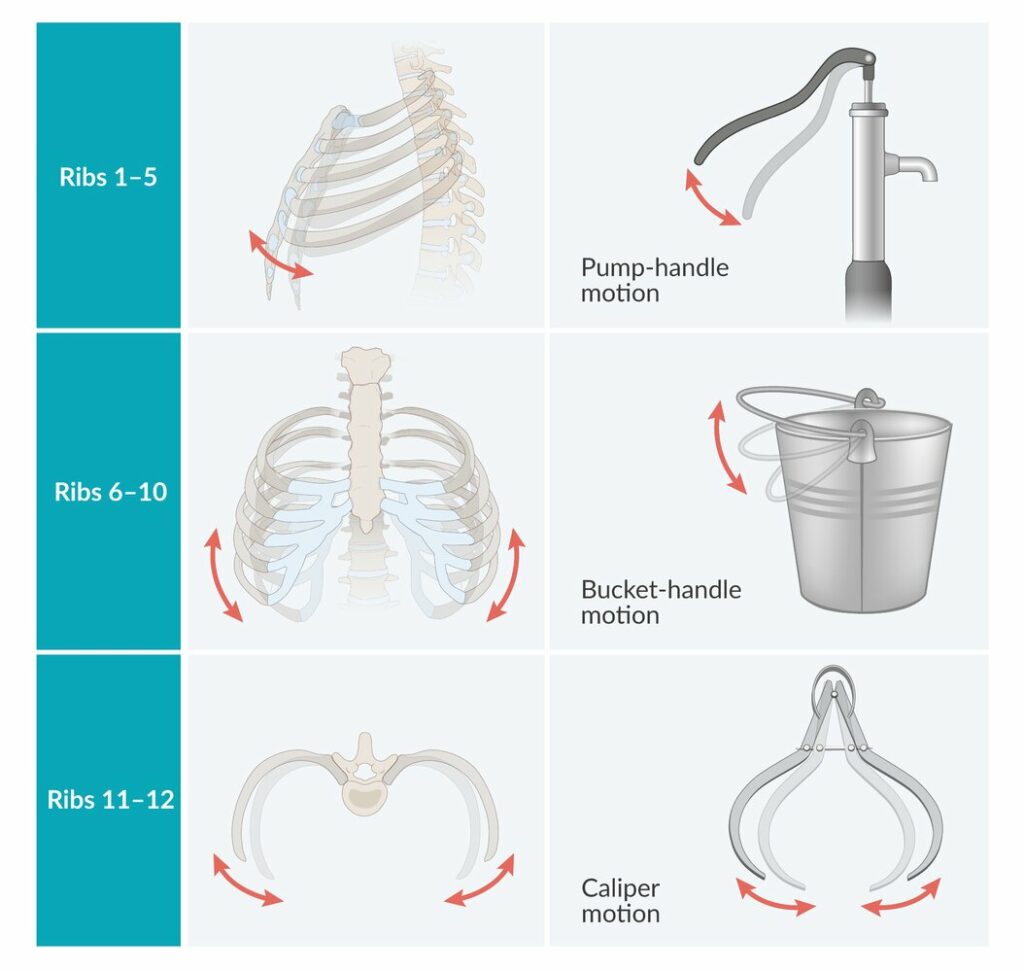
In my experience treating others with costochondritis, the thoracic spine is often overlooked. The ribs function like a bucket handle during respiration. If the handle attachment is stiff (i.e. where the ribs attach to in the upper back), then additional stress can occur where the ribs meet the breastbone. Therefore, treatment is targeted at the thoracic spine instead of where the symptoms are commonly felt.
Prognosis: Will It Go Away?
Most people with costochondritis recover fully within a few weeks, especially with conservative treatment. Studies have shown that 91% of patients see their symptoms resolve after three weeks of rest and NSAIDs.
While recurrence is possible, it’s relatively rare—only about 4% of patients experience a return of symptoms after two years.
In my case, my symptoms went away within a week after the emergency room visit. Total recovery time was about 4 weeks from initial symptoms onset. I followed a daily routine of thoracic mobility exercises to improve extension and rotation. I also prioritized my sleep and stress levels. I supplemented this routine with a few sessions of soft tissue and thoracic joint mobilizations with a physiotherapist.
Final Thoughts
If there's one piece of advice I would share with others who may be experiencing similar chest pain, it would be to seek medical attention right away. Even though costochondritis is not life-threatening, it's crucial to rule out more serious cardiac or pulmonary conditions first. With the right diagnosis and treatment plan, most people with costochondritis can find relief and return to their normal activities. It's a reminder that even seemingly minor health issues can have a significant impact on our day-to-day lives, but they can often be managed effectively with the right care and approach.

.png)
