Did you know that the human body has 320 skeletal muscle pairs? That’s 640 total working together to make us move, push and pull. It is amazing that we have the capability to synchronize these muscles, almost involuntarily, to produce the simple movements that we take for granted every day. Strengthening and improving the way that our musculoskeletal system functions has so many great benefits to our health and performance, and can substantially improve quality of life. The first step to that is determining your starting point — and that’s where we come in.
Assessing muscle strength is a key aspect of physical examination. When we evaluate muscle strength, what we are measuring is the maximum voluntary resultant output that the muscles can exert under a specific set of conditions.1 This output is typically the sum of the activation of a group of muscles and, therefore, is more appropriately the strength of the action being performed, rather than that of one individual muscle. The most common manner of doing so is measuring the peak, or maximum, force that can be generated during a single effort.

At Kinetic Labs, we use a custom-made fixed-frame isometric force dynamometer —the Force Bar. What does that mean? Let’s break it down. First, the Force Bar is a force dynamometer; which is an instrument that measures the torque — or rotational force — about different joints in the body. This force is measured isometrically, meaning that the body part of interest is set at a specific angle, and the strength of the muscles while in that position are measured. The device is fixed to a frame to ensure consistent and stable resistance to muscle force. And lastly, it is custom-made — designed exclusively for our team and specifically for what we need it to do.
Tests of muscle strength have been used for over a century, and methods continue to evolve.
Manual Muscle Testing (MMT) is a system in which the clinician applies manual resistance to an athlete’s movement in order to assess their strength. This method may involve the use of observation, palpation and force application by the clinician to determine the strength of a muscle action1. A score is then given to the athlete based on an ordinal grading system. MMT is one of the most common ways to assess muscle strength and weakness and is recognized as a subjective measure. 1-5 This system is reliant on the personal experience, skill, and strength of the clinician to administer and evaluate effectively.1,3-5 In addition to the ability to produce a matching force themselves to stabilize the athlete, the clinician also needs to have a sense for normative values of force as they relate to the sex, age, height and weight of the individual.3-5 Despite this, many studies have found MMT to show good reliability intra-rater and variable inter-rater reliability.3,6 This means that the clinicians have been able to reproduce a test score within their own grading system, however, comparing results between testers is less suitable.4,7 Due to the nature of this type of test, discrete changes in muscle strength might not be realized. An examiner may only be able to grade clinically detectable weakness, particularly in stronger muscle groups, and among individuals whose strength may not be impaired.1,3-5 Because MMT uses an ordinal scale, one single grade may correspond to a wide range of objectively measured strength7. Differences of 20-50% of maximum strength have been reported in some cases as indistinguishable using MMT.1,3 Limited sensitivity aside, manual muscle testing is a clinically versatile and practical tool which is inexpensive and time efficient to administer.5
What is handheld dynamometry?
Handheld Dynamometry (HHD) measures the peak isometric force generated from a muscle group.5 This procedure is pretty self-explanatory — the clinician holds the dynamometer in their hand, against the area being tested. The athlete would then exert force against the dynamometer while the clinician holds steady against their effort1. This method is more sensitive and specific in detecting mild weakness, as it is capable of capturing smaller strength differences than manual muscle testing.3,5 Using HHD also provides a more objective means of measuring muscle strength than manual muscle testing and uses a continuous range of torque values.3 Because handheld dynamometry is portable and easy to use, it allows for a wide variety of tests to be carried out in a time efficient manner, and is more ideal for clinical use.3,5,8 Additionally, hand-held dynamometry has demonstrated excellent reliability and good levels of concurrent validity.2-5,9-12 Similar to MMT, however, using a handheld dynamometer is reliant on the strength and skill of the clinician to stabilize the testing body.5,8 This issue challenges the achievable levels of validity and reliability, as the maximum force that can be measured may be limited by the strength of the clinician, and lack of stabilization of the participants and the device.1,13
What is isokinetic dynamometry?

Isokinetic dynamometry is regarded as the gold standard tool for measuring muscle strength in research settings.9 This computerized device allows for the measurement of dynamic strength of a muscle group throughout the joint’s entire range of motion.14 To do this, a mechanical arm is set to move at a constant velocity between a desired beginning and end point which represent the joint’s range of motion. So, for example, to measure the quadriceps strength of an athlete, they would sit in a seat and their leg would be strapped to the mechanical arm of the dynamometer. The clinician would adjust the machine to the athlete’s proportions and set the endpoints of the athlete’s range of motion. Starting at the maximum knee flexion angle, the athlete would be instructed to try and push the mechanical arm and extend their knee as hard as they can. The mechanical arm is programmed to rotate at a constant speed throughout the range of motion, and so no matter how hard they push, the athlete will only be able to extend their knee at that rate. The dynamometer then records the force output from the leg onto the mechanical arm to get the dynamic strength of the quadriceps muscle group. Isokinetic dynamometry is a reliable and valid tool for measuring isometric and isokinetic strength and is used as the comparison instrument for criterion validity of other muscle force measuring tools.5,9,14 This objective tool is commonly used in research settings, however, are large, lack portability and require time-consuming testing and training sessions, making them less ideal in terms of practicality for everyday use in a clinical setting.8,9,13
How do you test muscle strength at Kinetic Labs?
At our clinic, we are using the best and most suitable equipment for our use — the Force Bar. The Force Bar is a way to obtain an objective measure of muscle strength that is highly reliable, valid and practical for clinical use.9,13 By stabilizing the dynamometer using a fixed object, the validity and reliability of measurements from stronger muscle actions can be substantially improved in comparison to handheld dynamometry.1,8,9,13 In addition, measurements using fixed dynamometry have been shown to correlate significantly with those captured using isokinetic dynamometry, the gold standard in strength testing.1,8 Our Force Bar can be adjusted to measure any part of the body from a variety of angles isometrically, and is portable for convenient use inside and outside of the clinic. The applications for using this type of device are plentiful. Here’s why we believe it’s key for our assessments…

Injury Risk Prevention and Rehabilitation
Deficits in maximal strength are commonly reported following musculoskeletal injury.15 Identifying muscle weaknesses through strength testing in an assessment provides a baseline for clinicians to create a treatment plan, and subsequently evaluate its effectiveness over time.2 Some positive changes that athletes see by using this type of training include the strengthening of tendons and ligaments, improved muscular support to the joints and fatigue resistance to high loads.16 These benefits, to name a few, help to protect the body from injury.16 Recently, research has reported decreases in risk of overuse injury by up to 66% with the implementation of prescription methods that focus on strength training.15,16 When it comes to minimizing injury risk while simultaneously improving performance, there is no substitute for improving muscular strength.
Performance Measures
It is undeniable the positive influence that muscular strength has many aspects of athletic performance.16 Rate of force development, mechanical power, mobility, balance and coordination have all seen improvement in countless studies as a result of increased muscular strength.1,16,17 Whether you are jumping, sprinting or throwing, the benefits of achieving greater muscular strength differentiates performance and could determine the outcome of competition between athletes. In both strength-power and endurance sports, we see stronger athletes outperform their weaker counterparts. In fact, external power has been indicated as one of the main differences seen between the playing levels of athletes, and between starters and non-starters.16 It is expected that athletes seek to develop and improve muscular strength in an effort to translate to improved performance in sport. By measuring the muscular strength of athletes, we can gain the insights needed to make appropriate adaptations to training interventions, and give athletes the opportunity to realize their full potential.
Musculoskeletal Health
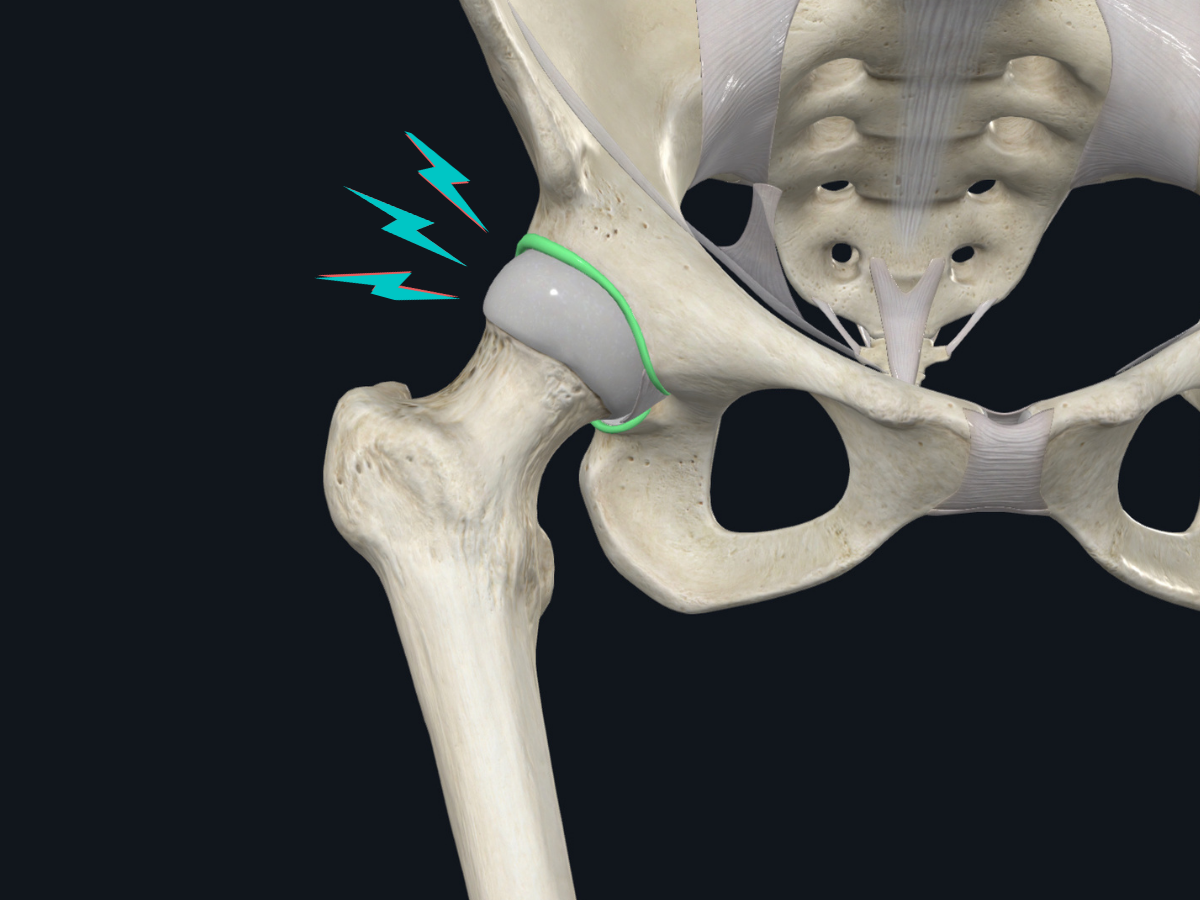
As we age, losses in muscle strength, balance and gait are associated with an increased risk of falls and fractures.1,17-19 Muscular strength is an important measure of these risks, and an indicator of the physical function in aging adults.8,13 Muscle weakness can be an indicator of several orthopaedic pathologies. For example, hip extensor weakness has been linked to low back pain and hip osteoarthritis.2 Our clinicians can then use these data to prescribe specific exercises to improve the way we move and actions we perform throughout each day. By using the Force Bar, we can detect mild deteriorations or improvements during the course of rehabilitation and training programs.3,5 This technology can assist our clinicians in making differential diagnoses, determining functional impairment, and planning therapeutic measures for recovery.3
References
- Bohannon, R.W. (2019). Considerations and Practical Options for Measuring Muscle Strength: A Narrative Review. BioMed Research International 2019.
- Keep, H. Luu, L., Berson, A. & Garland, S.J. (2016). Validity of the Handheld Dynamometer Compared with an Isokinetic Dynamometer in Measuring Peak Hip Extension Strength. Physiotherapy Canada 68(1), 15-22.
- Wadsworth, C.T., Krishnan, R., Sear, M., Harrold, J. & Nielsen, D.H. (1987). Intrarater Reliability of Manual Muscle testing and Hand-held Dynametric Muscle Testing. Physical Therapy 67(9), 1342-1347.
- Hayes, K., Walton, J.R., Szomor, Z.L. & Murrell, G.A.C. (2002). Reliability of 3 methods for assessing shoulder strength. Journal of Shoulder and Elbow Surgery 11(1), 33-39.
- Pfister, P.B., de Bruin, E.D., Sterkele, I., Maurer, B., de Bie, R.A. & Knols, R.H. (2018). Manual muscle testing and hand-held dynamometry in people with inflammatory myopathy: An intra- and interrater reliability and validity study. PLoS ONE 13(3).
- Cuthbert, S.C. & Goodheart Jr, G.J. (2007). On the reliability and validity of manual muscle testing: a literature review. Chiropractic & Osteopathy 15(4).
- Symonds, T., Campbell, P. & Randall, J.A. (2017). A Review Of Muscle- And Performance-Based Assessment Instruments In DM1. Muscle & Nerve 56, 78-85.
- Kim, W.K., Kim, D., Kyung, M.S. & Kang, S.H. (2014). Reliability and Validity of Isometric Knee Extensor Strength Test With Hand-Held Dynamometer Depending on Its Fixation: A Pilot Study. Annals of Rehabilitation Medicine 38(1), 84-93.
- Bui, K., Mathur, S., Dechman, G., Maltais, F. Camp, P. & Saey Didier (2019). Fixed Handheld Dynamometry Provides Reliable and valid Values for Quadriceps Isometric Strength in People With Chronic Obstructive Pulmonary Disease: A Multicenter Study. American Physical Therapy Association 99(9), 1255-1267..
- Lee, C. (2019). Validity of hand-held dynamometer in assessing isometric leg strength in older adults. International Journal of Applied Sports Sciences 31(1), 52-57.
- Seko, T., Mori, M., Ohnishi, H., Himuro, N., Takahashi, Y., Kumamoto, T., Ito, T. (2018) Reliability and Validity of Seated Hip Extensor Strength Measurement by Handheld Dynamometer in Older Adults. Journal of Geriatric Physical Therapy 42(4), 39-44.
- Liberatori Junior, R.M., Netto, W.A, Carvalho, G.F., Zanca, G.G., Zatiti S.C.A. & Mattiello, S.M. (2019). Concurrent validity of handheld dynamometer measurements for scapular protraction strength. Brazilian Journal of Physical Therapy 23(3), 228-235.
- Sung, K., Yi, Y.G. & Shin, H. (2019) Reliability and validity of knee extensor strength measurements using a portable dynamometer anchoring system in a supine position. BMC Musculoskeletal Disorders 20(320).
- Drouin, J.M., Valovich-mcLeod, T.C., Shultz, S.J., Gansneder, B.M. & Perrin, D.H. (2004). Reliability and validity of the Biodex system 3 pro isokinetic dynamometer velocity, torque and position measurements. European Journal of Applied Physiology 91, 22-29.
- Lauersen JB, Bertelsen DM & Andersen LB (2014) The effectiveness of exercise interventions to prevent sports injuries: a systematic review and meta-analysis of randomized controlled trials. British Journal of Sports Medicine 48, 871-877.
- Suchomel, T.J., Nimphius, S. & Stone, M.H. (2016). The Importance of Muscular Strength in Athletic Performance. Sports Medicine 46, 1419-1449.
- King, G.W., Abreu, E.L., Kelly, P.J. & Brotto, M. (2019). Neural control of postural sway: Relationship to strength measures in young and elderly adults. Experimental Gerontology 118, 39-44.
- Daly, R.M., Rosengren, B.E., Alwis, G., Sembro, I. & Karlsson, M.K. (2013). Gender specific age-related changes in bone density, muscle strength and functional performance in the elderly: a 10-year prospective population-based study. BioMed Central Geriatrics 13:71.
- Neje, S., Loefler, S., Cvecka, J., Sedliak, M.& Kern. H. (2013). Strength training in elderly people improves static balance: a randomized controlled trial. European Journal Translational Myology - Basic Applied Myolohy 23(3), 85-89.



.png)
