What is mechanical low back pain?
Mechanical low back pain is common. Over 50% of adults will experience it at some point in their lives. Pain typically occurs between the ages of 20 to 65, though it is less common in those ages 20 – 35. Even school-aged children can experience mechanical lower back pain.
Functionally, the low back area, more formally called the lumbar area, supports the weight of the upper body while providing flexibility and movement to the trunk region. The lumbar spine itself also serves to protect the spinal cord and nerves within the vertebral canal.
Pain in this area can originate from conditions affecting:
- Lumbar spine
- Intervertebral discs
- Ligaments surrounding the spine and discs
- Spinal cord and nerves
- Muscles of the low back
- Internal organs of the abdomen and pelvis
- Skin covering the lumbar area
Anatomy of the lower back and spine
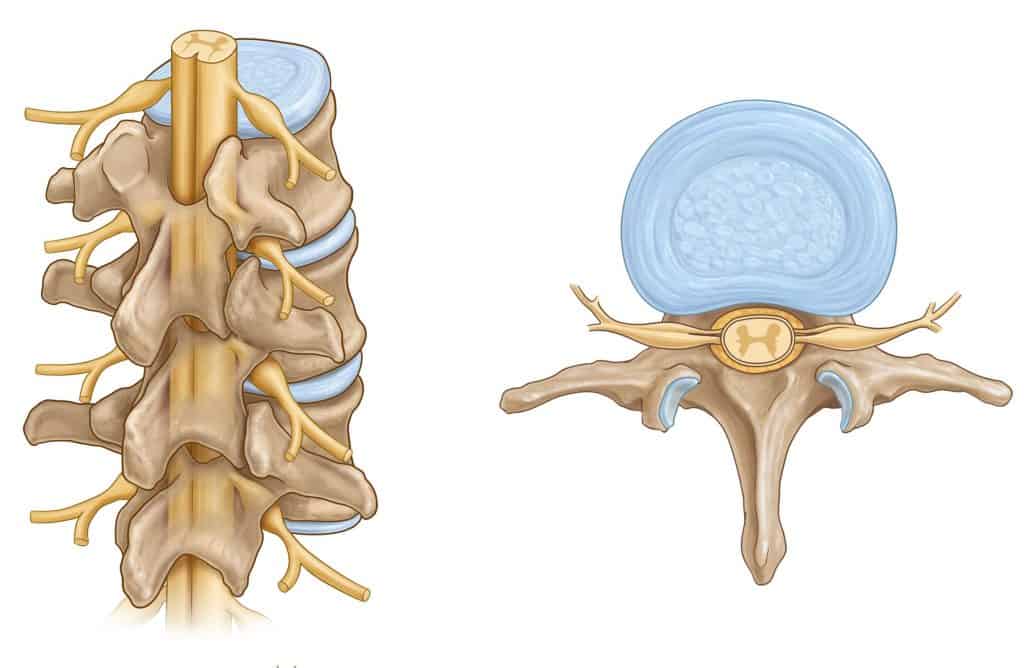
The lumbar spine is designed so vertebrae stack together. This provides a movable support structure while protecting the spinal cord from injury. The spinal cord is composed of nervous tissue that extends down the vertebral canal from the brain. Nerves branch off the spinal cord and transmit signals to and from the brain.
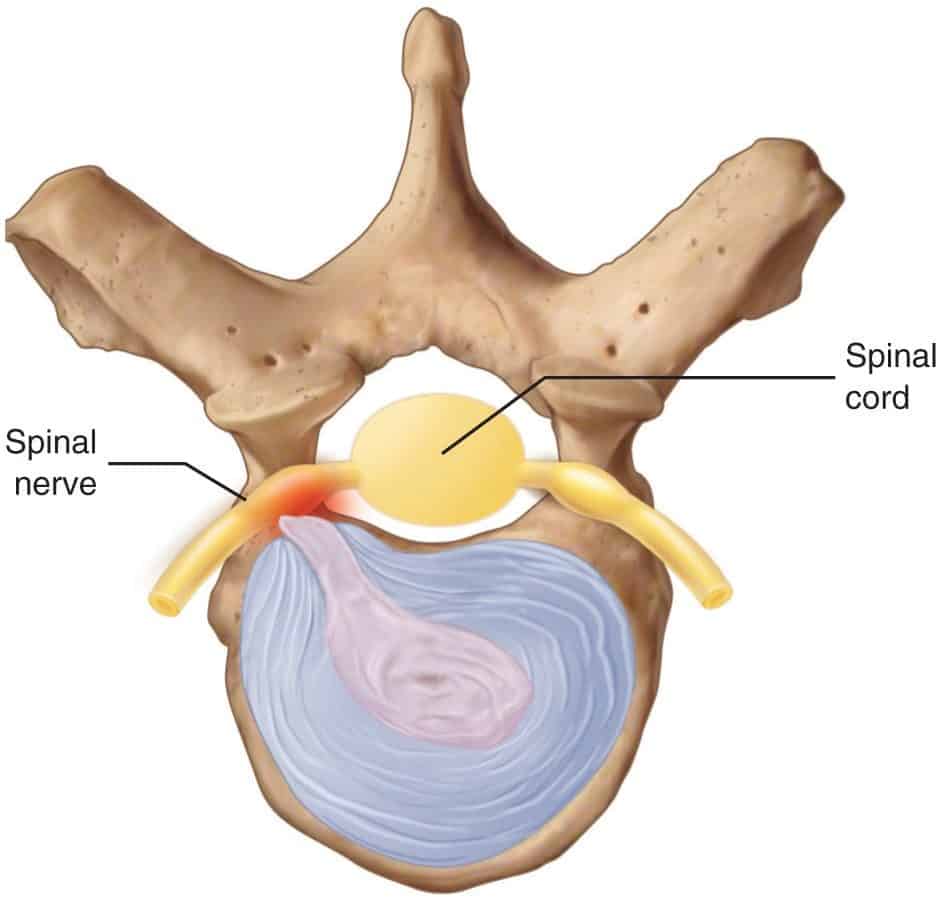
Between the vertebrae are intervertebral discs that act as shock absorbers to minimize forces on the spinal column. Each disc is designed like a jelly donut, with a soft central nucleus pulposus and an outer firm annulus fibrosis. The jelly is capable of rupturing. This is called a disc herniation. Pain from a disc herniation occurs when the central nucleus pulposus rubs against adjacent nervous tissue causing irritation.
Ligaments are strong band-like fibrous tissue that attaches bone to bone. In the lumbar area, ligaments attach the vertebrae to one another. All muscles attach to bones via tendons.
Muscles that are responsible for the trunk’s movement, such as bending forward and backward, as well as some lower limb movements, attach to the lumbar spine. These muscles receive signals from the lumbar nerves to move.
Vital pelvic organs include the uterus and ovaries in women and the prostate in men. The kidneys lay on either side of the lumbar spine.
Major blood vessels that transport blood to and from the lower limbs pass just in front of the lumbar spine. Along with it are lymph nodes (important in the immune response) and tissues of the involuntary nervous system that maintain bladder and bowel control.
The skin over the lumbar spine sends signals, such as pressure, temperature, and pain, to the brain via nerves. Most of the structures mentioned above are also capable of sending pain signals to the brain, potentially contributing to low back pain.
What are the different types of low back injuries?
Low back pain can be divided, by cause, into three categories:
- Mechanical: sprains, strains, disc herniations, arthritis
- Non-mechanical: tumor, infection, inflammatory arthritis
- Visceral: originating from the internal organs
Over 95% of low back pain cases fall into the category of mechanical.
Low back injuries can then be subdivided by time frame. These time frames include acute (lasting less than four weeks), subacute (lasting 4 to 12 weeks), and chronic (lasting more than 12 weeks).
The vast majority of those with mechanical low back discomfort will recover within six weeks. Although, it’s important to note that recurrence is common. About 30% will go on to have chronic back pain, meaning pain of at least a moderate intensity one year after an acute episode.
What are specific diagnoses of back pain?
Lumbar strains/sprains – injuries to the tendons and ligaments are called strains and sprains respectively, 70% of all mechanical low back injury cases are strains or sprains.
Spondylosis – arthritis of the spine.
Disc herniation/discogenic pain – a disc herniates when the “jelly” or nucleus pulposus ruptures through the outer ring called the annulus fibrosus. Tearing of the annulus fibrosis, which may or may not precede a disc herniation can cause discogenic pain.
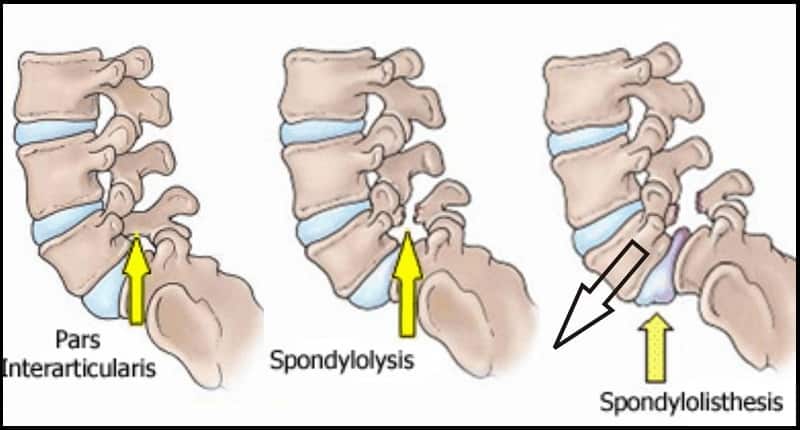
Spondylolysis/Spondylolisthesis – Rarely a fracture can occur through the pars interarticularis, the thin portion of the vertebrae that connects their joints. The pars interarticularis is the weakest point of the vertebra. While a spondylolysis can occur at any age, it is most common in children and adolescents. A spondylolysis can weaken the vertebra to such an extent it is unable to maintain its proper position and shifts forward, called a spondylolisthesis.
Vertebral fracture – fractures can occur over time or with trauma.
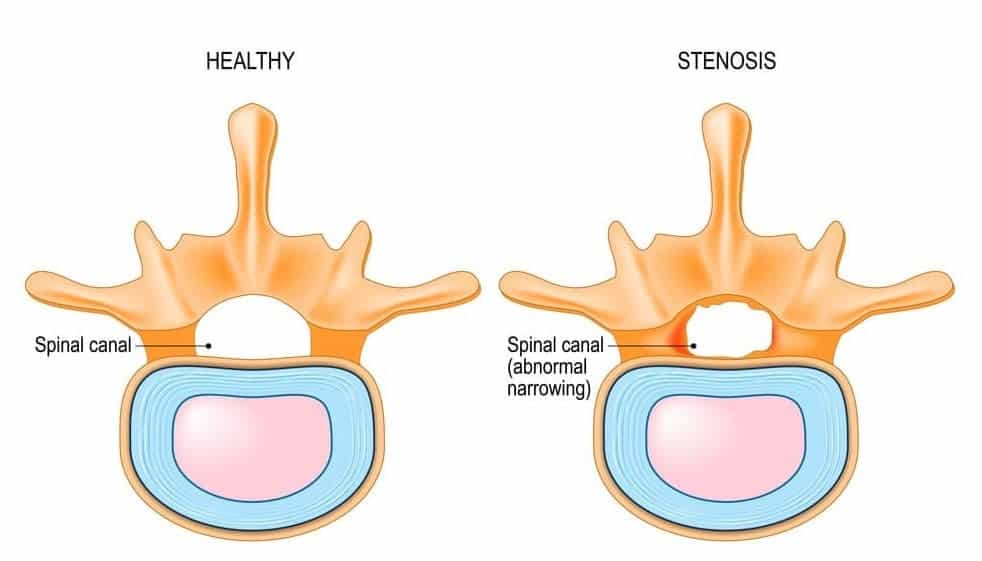
Spinal stenosis – narrowing of the spinal canal, putting pressure on its contents, the spinal cord and nerves.
Sacroiliac joint pain – low back pain can cause pain into the buttocks and upper thighs.
Who is more likely to get mechanical low back pain
Obesity – mechanical low back is more common in those with a high BMI. Greater mechanical stress placed on the lumbar spine by the increased weight is thought to be the cause.
Stress and psychiatric comorbidities – stress and psychiatric disorders such as anxiety and depression have been shown to increase the likelihood of mechanical low back pain becoming chronic.
Older age – the increased prevalence of mechanical low back pain with age can be explained by wear and tear and degenerative changes.
Previous low back injury – recurrence is common.
Heavy physical and occupational activities – both acute and repetitive injuries can occur in the low back with these activities.
How is mechanical low back pain diagnosed?
Mechanical low back pain is diagnosed through a combination of history taking, physical examination, and imaging (if necessary). Though, most cases of back pain do not require imaging.
The complexity and biomechanics (how the area moves) of the lumbar area often make it challenging to identify a specific anatomical cause, with a precise diagnosis made in only 20% of cases.
Imaging does not increase this percentage and may lead to unnecessary exposure to radiation.
How is mechanical low back pain treated?
Most cases of mild mechanical lower back discomfort resolve on their own and do not require treatment. When treatment is needed, pain is often treated, moving from simple, low-cost to more aggressive approaches.
Medications designed to relieve pain and or inflammation may be prescribed, such as analgesics, non-steroidal anti-inflammatory drugs (NSAIDs) or topical creams.
Conservative care aims to treat pain without the use of surgery. These approaches include massage, acupuncture, physical therapy, or spinal manipulation.
There are also psychological approaches to consider. Psychological options include cognitive behavioural therapy to address negative thinking patterns associated with pain, the development of pain-coping strategies, and practicing relaxation skills.
Surgery is also considered when other treatments fail. But surgery is only used in rare cases or emergencies.
How can you prevent lower back discomfort?
Exercise is the best defense against both the first episode of back pain and reoccurrence once an episode has been experienced.
Conclusion
- Mechanical low back pain is common - over 50% of adults will experience it in their lifetime
- It is usually caused by the structures of the lower back, not including organs - over 95% of cases are mechanical
- Pain can be acute (lasting less than four weeks) or chronic (lasting more than 12 weeks)
- Most cases will recover within six weeks
- About 70% of cases of mechanical low back pain are strain (tendon or muscle injuries) or sprains (ligament injuries)
- Due to the complexity and biomechanics of the lumbar area, a specific diagnosis often cannot be made – only about 20% of cases get an accurate diagnosis
- Exercise is helpful in the prevention lower back injuries
References
- Evaluation and Diagnosis of Low back pain. E, Manusov. 2012. https://pubmed.ncbi.nlm.nih.gov/22958556 Musculoskeletal Lower Back Pain. BMJ Best Practice. 2018. https://bestpractice.bmj.com/topics/en-us/834 Mechanical Low Back Pain. J. Will et. all. 2018. https://www.aafp.org/afp/2018/1001/p421.html Low Back Pain Fact Sheet. National Institute of Neurological Disorders and Stroke. 2020. https://www.ninds.nih.gov/Disorders/Patient-Caregiver-Education/Fact-Sheets/Low-Back-Pain-Fact-Sheet


.png)
