A humerus fracture refers to a break or crack in the humerus, which is the long bone of the upper arm. The humerus extends from the shoulder joint to the elbow joint and is an essential component of the skeletal system. Fractures of the humerus can occur in various locations along the bone, and they can be classified based on factors such as the specific part of the bone affected and the nature of the fracture.
Common types of humerus fractures include:
Proximal Humerus Fracture: This type occurs near the shoulder joint at the top of the humerus. It may involve the anatomical structures associated with the shoulder, such as the head of the humerus or the greater tuberosity.
Shaft Humerus Fracture: This involves a break in the midsection (shaft) of the humerus. The shaft is the long, straight part of the bone between the shoulder and the elbow.
Distal Humerus Fracture: This type occurs near the elbow joint, involving the lower end of the humerus. Fractures in this region can affect the condyles (rounded projections at the end of the bone) or other structures.
Humerus fractures can result from various causes, including trauma, falls, sports injuries, or motor vehicle accidents. The severity of the fracture can range from a simple crack to a more complex break with multiple fragments. Treatment depends on factors such as the type and location of the fracture, as well as the individual’s overall health. Common treatment options include casting, splinting, or surgical intervention to realign and stabilize the fractured bone.
The symptoms of a humerus fracture can vary depending on the location and severity of the fracture. Common signs and symptoms may include:
Pain: Pain is a typical symptom of a humerus fracture. The intensity and location of the pain can vary, but it is often localized to the site of the fracture.
Swelling: Swelling around the injured area may occur, as the body responds to the trauma and inflammation.
Bruising: Bruising (ecchymosis) may develop around the fracture site due to bleeding under the skin.
Deformity: In some cases, a visible deformity or an abnormal arm alignment may be apparent, especially with more severe fractures.
Limited Range of Motion: The ability to move the arm may be restricted, and any attempt may cause pain.
Tenderness to Touch: The affected area may be tender to the touch, and there may be increased sensitivity.
Numbness or Tingling: Severe fractures or fractures involving nerve damage may lead to numbness or tingling in the affected arm.
Previous studies have proposed certain risk factors for proximal humerus fractures. These include diminished bone mass and related factors like height loss since the age of 25, a personal history of fractures, a maternal history of hip fractures, low levels of physical activity, and a low body mass index (BMI). It’s worth noting that one study did not establish a correlation with low BMI. Interestingly, menopausal hormone therapy has been identified as a protective factor against proximal humerus fractures.
Another study found that the single biggest risk factor for secondary displacement (i.e. the fracture shifts and bones move) of a proximal humerus fracture is age above 65 years old.
Proximal humerus fractures are classified based on the Mayo-FJD classification, which describes 7 common fracture patterns that each have different outcomes when treated without surgery.
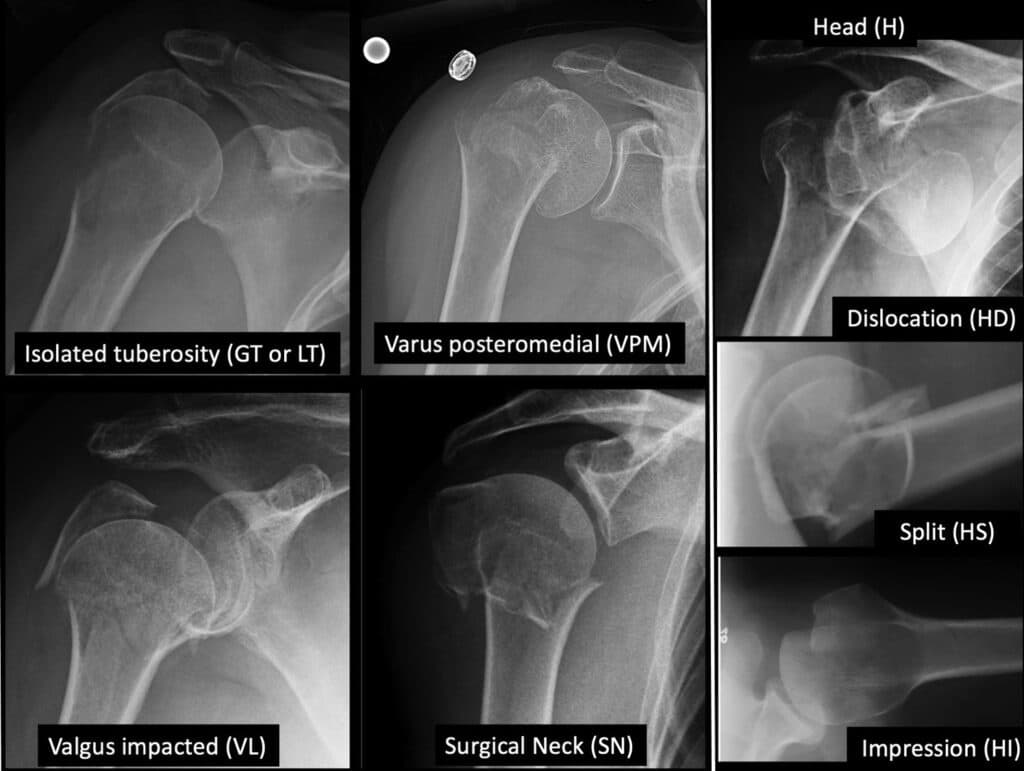
Fractures of the Greater Tuberosity or Lesser Tuberosity
Fractures of the Greater Tuberosity (GT) or Lesser Tuberosity (LT) may occur with or without shoulder dislocation. Nonoperative treatment risks impingement or rotator cuff dysfunction, particularly if displaced.
Fractures with Severe Head Compromise
Fractures involving severe head compromise, such as head dislocation (HD), head splitting (HS), or head impaction (HI), may lead to persistent instability, maltracking, and osteoarthritis. Surgery is usually recommended due to these anticipated complications.
Varus Posteromedial Fractures
Varus posteromedial (VPM) fractures involve comminution and collapse at the posteromedial neck-head junction, potentially resulting in malunion if untreated. Nonunion is rare due to bony impaction, and adverse outcomes include decreased range of motion and loss of function.
Valgus Fractures
Valgus (VL) fractures displace the humeral head in a valgus direction, and the greater tuberosity is almost always fractured (VL-GT). Malunion is a potential adverse outcome, with added instability if the medial periosteal hinge is disrupted. Avascular necrosis may occur with nonsurgical treatment.
Surgical Neck Fractures
Surgical neck (SN) fractures occur at the metaphyso-diaphyseal junction, separating the head and tuberosities from the diaphysis. Lack of impaction distinguishes SN fractures from VPM and VL fractures. Nonoperative treatment risks nonunion, especially with substantial displacement or compromised healing potential.

The non-operative treatment of proximal humerus fractures (PHF) typically involves initial immobilization followed by physiotherapy. Immobilization provides support and pain relief during healing, while physiotherapy focuses on restoring function and mobility. It is recommended to immobilize PHF in external rotation, especially for surgical neck fractures or those involving a greater tuberosity fragment. Immobilizing the shoulder with the arm resting on the patient’s belly may lead to internal rotation malunion for humeral neck fractures.
The duration of shoulder immobilization is usually 3 to 4 weeks, balancing fracture stability and healing progress. Prolonged immobilization, particularly in elderly patients, can impact independence and result in stiffness and pain. Early mobilization strategies have shown promising outcomes, with studies indicating faster recovery, less pain, and better function, especially in stable fractures with impaction. Some studies have compared outcomes based on different immobilization periods, with evidence suggesting that shorter immobilization durations, such as 1 week, may yield similar functional results as longer periods, independent of fracture complexity. However, further research is needed to assess long-term outcomes beyond the 6- to 24-month follow-up periods studied so far.
In our accelerated rehabilitation protocol, we encourage you to engage in activities of daily living for self-care and hygiene after 1 week, with the sling being removed during rest and physical therapy exercises. Codman pendulum exercises for passive shoulder range of motion can begin immediately, followed by passive forward elevation exercises from the third to fourth week. Active assisted range of motion exercises may be introduced at 6 weeks, and strengthening exercises can commence at 3 months post-injury. You can perform the exercise program at least twice daily for 10 to 15 minutes each time.
In isolated greater tubercle fractures, we can sometimes accelerate this timeline even further depending on your response to treatment. The rehabilitation protocol for weeks 1 to 6 involves initial immobilization of the fracture, however, Codman pendulum exercises and active movement for the elbow, wrist, and hand in week 1 are allowed. In week 2, patients progress to active assisted exercises, including assisted flexion with the opposite hand or the use of a stick for assistance. Weeks 3 to 6 focus on active assisted exercises such as flexion and abduction exercises using a wall, pulley exercises with a towel over a door, and the introduction of light weights for pendulum exercises.
Weeks 4 to 6 mark the initiation of assisted rotations, including rotations in adduction and abduction using self-assistance, a stick, or a towel. Weeks 7 to 10 introduce active nonresisted and isometric exercises, including isometric exercises leaning on a wall and compressing a ball between both hands. Pushups on a wall are also incorporated. From week 11 onwards, resisted exercises are introduced, including exercises with elastic bands for flexion, abduction, adduction, and progressive rotations.
Conservative treatment for non-displaced or minimally displaced impacted proximal humerus fractures (PHF) generally results in favorable outcomes for 80% to 90% of patients. However, more complex or displaced fractures may lead to worse outcomes after conservative treatment. One study found that one-part fractures had better outcomes compared to displaced fractures, with four-part fractures demonstrating the poorest functional results. Despite limited functional outcomes in displaced PHF, subjective quality of life perception did not significantly differ between displaced and non-displaced fractures, possibly due to the influence of an older population where range of motion mattered less.
For elderly patients with limited functional expectations, non-operative treatment might be appropriate as it provides good pain relief, although with limited function. Results of conservative treatment are influenced by factors such as fracture displacement, patient age, and fracture pattern. In active patients, surgical treatment may be considered to avoid complications such as nonunion, malunion, and avascular necrosis associated with non-operative treatment. The complications can impact shoulder function, and avascular necrosis, in particular, may vary in severity but often results in minimal symptoms. Surgical intervention may be necessary for certain fracture situations associated with an increased risk of avascular necrosis, especially in cases where anatomical fracture healing is not achieved.