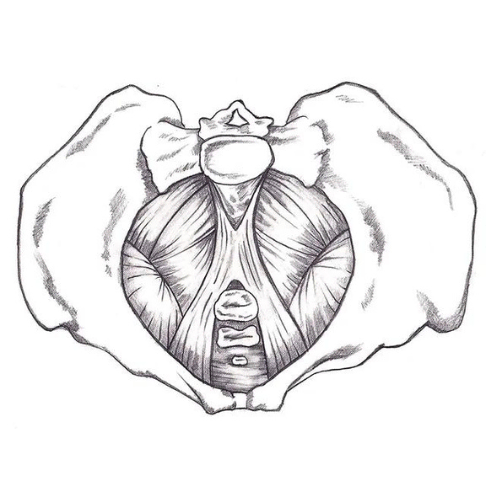
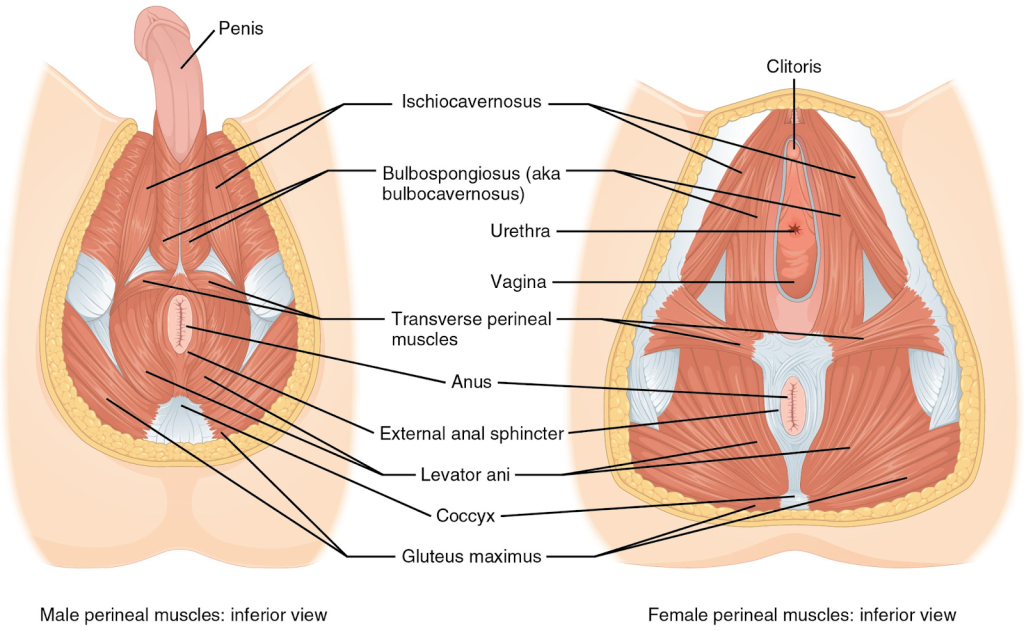
The pelvic floor is a group of muscles, connective tissue, and bone attachments in your pelvis. These muscles are part of your ‘core’ and work with other muscles to provide both stability and movement. The pelvic floor also helps to maintain bowel and bladder control, pelvic organ support, lymphatic and blood flow, and sexual function.
Everyone has a pelvic floor (including men), and can experience incontinence, pelvic pain or dysfunction at any stage of life. While the stigma surrounding pelvic health is slowly dissipating, many people endure symptoms for many years before seeking medical help, or attribute their symptoms to normal aging. While is very common that people experience urine leakage or pelvic dysfunction as they age, it is not normal and should be addressed.
Certain instances that may affect how the pelvic floor is functioning include:
Common signs of a pelvic floor issue include:
Pelvic Health Physiotherapy includes assessment and treatment of the muscles, nerves, joints and connective tissue of the pelvis and surrounding areas. Your assessment may include a vaginal and/or rectal exam. If you had physiotherapy for your knee, you would expect your physiotherapist to inspect and touch your knee to diagnose the issue. This is the same with the pelvic area, however since most of the muscles are inside your pelvis, an internal exam is the best way to assess them. Ultimately, what exams are performed during your assessment will be determined based on your specific issue, goals, and comfort level.
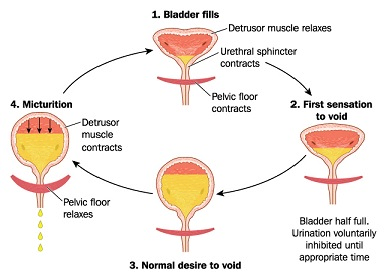
Incontinence
Approximately 3.3 million Canadians are affected by at least one type of incontinence.1 The most common types of incontinence are stress (leaking with jumping, running, sneezing, etc.), urge (inability to make it to the toilet on time), or a mix of both. Overflow incontinence can also occur, which is when the bladder fills beyond its capacity and the excess urine dribbles out. There has been ample research conducted for stress and urge incontinence and pelvic floor muscle training is recommended as first-line conservative treatment.2 This can include working on the strength, relaxation, endurance, and power of the muscles.
Can I just do kegels?
Pelvic floor dysfunction can be caused by hypotonicity (weak pelvic floor muscles), hypertonicity (tight pelvic floor muscles), or both. While kegels can be helpful for some people with weak pelvic floors, they can exacerbate symptoms for those with tight pelvic floors. As well, kegels are often not performed correctly, and in this case will not help with strengthening. A physiotherapy assessment can determine if kegels are a good exercise for you, and ensure that you are performing them correctly.
Lumbopelvic pain
Low back pain is the leading cause of disability worldwide, and is most prevalent in women aged 40-80 years old.3 With the female population, research has found a link between low back pain and pelvic floor dysfunction. One study investigating 200 women aged 17-45 with low back pain, urinary incontinence was reported by 78%.4 Another study looking at pelvic floor dysfunction in women with low back pain (85 women with a mean age of 43), found 95% had pelvic floor muscle tenderness during a vaginal exam, and 65% had pelvic floor muscle weakness.5 Pelvic floor muscle tenderness can indicate increased tension and decreased ability to relax the muscles. Since the pelvic floor plays a role in maintaining intra-abdominal pressure and support of the lumbopelvic area, it is important to address pelvic floor dysfunctions in those presenting with low back pain.
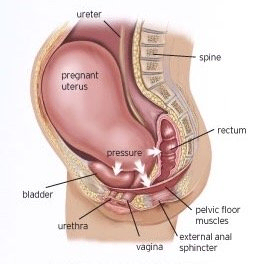
Pregnancy/Postpartum
Women’s bodies undergo many changes during pregnancy, labour, and post-partum. There are many ways that pelvic health physiotherapy can help.
Vaginal exams can safely be performed during your second and third trimester, unless your physician has recommended that you abstain from intercourse.
Vaginal exams can safely be performed at six weeks postpartum, or once you have been cleared by your physician.
Pelvic pain and dysfunction
Some of the most commonly diagnosed conditions in the pelvic area include:
There can be many different contributors to pelvic pain and dysfunction, including tense muscles, irritation to the nerves or skin, changes in hormones, and sensitization of the nervous system. With pain, it is important to address all factors that may contribute (including sleep, stress, fear, etc.), as well as the local tissues.